What Is Ischemia and Stroke? A Medical Guide to Brain Blood Flow Disorders
By Dr. Ellia Ciammaichella, DO, JD — Triple Board-Certified in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine
Quick Insights
Ischemia and stroke are directly connected medical conditions involving blood flow restriction. Ischemia is the broad medical term for reduced blood flow to any tissue or organ, causing oxygen deprivation. When ischemia affects the brain, it can cause a stroke—a medical emergency where brain cells die from lack of blood and oxygen. Ischemic strokes account for about 87% of all strokes and occur when blood clots block arteries leading to the brain. Common causes include atherosclerosis (plaque buildup), blood clots, and severe low blood pressure. Recognizing stroke symptoms and seeking immediate medical care is critical for preventing permanent brain damage.
Key Takeaways
- Ischemic strokes account for about 85% of all strokes, making them the leading type globally.
- Reduced blood flow during ischemia triggers brain cell damage within minutes, often leading to weakness, speech problems, or confusion.
- Major risk factors include high blood pressure, heart disease, smoking, and poorly controlled diabetes.
- Prompt therapies—like clot removal or medication—significantly improve recovery when started early after symptoms appear.
Why It Matters
Understanding ischemia and stroke empowers you to recognize warning signs, act quickly, and reduce long-term impacts on both daily living and legal rights. Immediate response not only safeguards your health, but ensures fair access to expert medical and legal support when outcomes are at stake.
Introduction
As a triple board-certified physician and attorney, I approach ischemia and stroke from both rigorous clinical and critical legal standpoints. Learn more about Dr. Ellia Ciammaichella’s unique dual qualifications (DO/JD) here.
Ischemia and stroke describe a sudden reduction in blood flow, typically caused by an arterial blockage, that quickly leads to brain cell injury and—if left untreated—long-term neurological deficits. Medically, this is among the most time-sensitive emergencies; legally, it raises complex questions if delays, misdiagnosis, or inadequate documentation affect patient outcomes, insurance, or even litigation.
Most strokes—about 85%—are classified as ischemic, making them the predominant form worldwide. Medical evidence underscores how rapid loss of brain perfusion leads to substantial impairment, meaning every minute counts for both recovery and subsequent evaluation of damages.
Understanding the intersection of prompt care, research, and accurate documentation is essential—whether you are a concerned patient, family member, or legal professional seeking clarity about the real-world stakes of ischemia and stroke.
Understanding Ischemia and Stroke
Ischemia and stroke are terms that describe a critical reduction in blood flow to the brain, resulting in tissue injury. Cerebral ischemia (reduced blood flow to brain tissue) is the underlying process in most strokes, particularly ischemic strokes, which account for the vast majority of cases.
In my experience, the distinction between ischemic and hemorrhagic stroke is essential for both immediate management and long-term prognosis. From my perspective as a triple board-certified physiatrist, I find that clarifying these terms at the outset equips both medical and legal professionals with a shared understanding when complex stroke cases are under review.
Defining Cerebral Ischemia
Cerebral ischemia occurs when an artery supplying the brain becomes blocked, depriving brain cells of oxygen and nutrients. This process can lead to irreversible cell death within minutes. I have seen that even brief interruptions in blood flow can result in significant neurological deficits, underscoring the urgency of rapid intervention.
Types of Stroke (Ischemic vs. Hemorrhagic)
There are two primary types of stroke: ischemic stroke (caused by arterial blockage) and hemorrhagic stroke (caused by bleeding into the brain). Ischemic strokes are far more common, representing about 85% of all cases. Hemorrhagic strokes, while less frequent, often result in more severe outcomes. Understanding these differences is crucial for both clinical care and legal analysis of causation and damages.
What is the Connection Between Ischemia and Stroke?
How does ischemia cause stroke?
Ischemia leads to stroke when a blocked artery prevents blood from reaching brain tissue, causing rapid cell injury and loss of function. This process is the primary mechanism behind most strokes.
The link between ischemia and stroke is direct: when blood flow is interrupted, brain cells begin to die, resulting in neurological symptoms such as weakness, speech difficulties, or confusion. In my dual role as a physician and legal consultant, I have found that timely recognition and documentation of this connection are critical for both patient outcomes and accurate damage assessment.
According to systematic reviews of global stroke guidelines, early intervention is the most important factor in reducing long-term disability. In my 15+ years of practice evaluating individuals with spinal cord and brain injuries, I’ve found that detailed functional assessment, beyond basic diagnosis, is essential for accurately delineating damages in legal proceedings.
When assessing stroke cases for both plaintiffs and defendants, precision in documenting the onset and severity of ischemic injury is vital for fair adjudication and appropriate care planning.
Common Causes and Risk Factors
The most common causes of ischemia and stroke include arterial blockages from blood clots, atherosclerosis (plaque buildup), and heart conditions such as atrial fibrillation. Major risk factors are high blood pressure, diabetes, smoking, high cholesterol, and a history of transient ischemic attack (TIA). In my practice, I have observed that addressing these risk factors can dramatically lower the likelihood of stroke.
It is important to note that some risk factors, such as age and genetics, cannot be modified, but many others can be managed through lifestyle changes and medical therapy. Recent research highlights the global burden of ischemic stroke and the need for aggressive risk factor management to prevent first and recurrent events.
Can Ischemia-Related Strokes Be Prevented?
What are the top ways to prevent ischemia-related stroke?
– Control high blood pressure
– Manage diabetes and cholesterol
– Quit smoking
– Exercise regularly
– Take prescribed medications as directed
Prevention of ischemia and stroke relies on both primary and secondary strategies. Primary prevention targets individuals who have never had a stroke, while secondary prevention focuses on those with a history of TIA or stroke. In my experience, a combination of medical therapy, lifestyle modification, and patient education yields the best results.
Having worked with hundreds of spinal cord injury cases, I’ve found that accurate functional assessment and documentation are equally valuable for plaintiffs seeking fair compensation and defendants requiring objective analysis. That same careful approach to evaluating and explaining risk factors—both modifiable and non-modifiable—supports robust prevention efforts and ensures readers understand their personalized risk profile.
Primary Prevention Strategies
Primary prevention involves controlling blood pressure, managing diabetes, maintaining a healthy weight, and avoiding tobacco. I emphasize to my clients that even modest improvements in these areas can significantly reduce stroke risk. Current guidelines recommend a multifaceted approach that includes both medication and lifestyle changes.
From my unique perspective with both medical and legal training, I can translate complex medical findings into precise documentation that clearly establishes functional limitations for both plaintiff and defense teams.
Secondary Prevention After TIA or Stroke
For those who have already experienced a TIA or stroke, secondary prevention is critical. This may include antiplatelet or anticoagulant medications, cholesterol-lowering drugs, and sometimes surgical interventions. Remote ischemic conditioning (RIC)—a technique involving brief, controlled periods of reduced blood flow to a limb—is being investigated for its potential to improve outcomes in stroke patients.
While some practitioners may overlook newer modalities like RIC due to unfamiliarity, I find that staying up to date with these advances can make a tangible difference in long-term outcomes, especially for those with high recurrence risk.
Symptoms, Diagnosis, and When to Seek Help
Recognizing the symptoms of ischemia and stroke is vital for prompt treatment. Common signs include sudden weakness or numbness (especially on one side), difficulty speaking or understanding speech, vision changes, severe headache, and loss of coordination. In my clinical and legal work, I stress that early diagnosis not only improves outcomes but also ensures accurate documentation for subsequent evaluation.
Diagnosis typically involves a neurological examination, brain imaging (CT or MRI), and blood tests. Timely and thorough documentation is essential for both medical management and legal review of potential damages.
When to Seek Medical Attention
Seek immediate medical attention if you experience:
- Sudden weakness or numbness on one side
- Difficulty speaking or understanding speech
- Sudden, severe headache
Prompt evaluation by a physician is critical to minimize brain injury and optimize recovery.
Treatment Options and Recent Advances
Treatment for ischemia and stroke has advanced significantly in recent years. The mainstays of acute therapy are intravenous thrombolysis (clot-busting medication) and endovascular thrombectomy (mechanical clot removal).
Remote ischemic conditioning (RIC) is being explored as a potential therapy to improve functional outcomes in stroke patients, though clinical trial results have been mixed. Comparative expertise matters here: While some medical experts focus solely on diagnosis, my approach emphasizes comprehensive functional assessment that provides all parties—physicians, attorneys, and litigants—with clear, accessible documentation of impairments. This approach ensures that both the medical team and legal stakeholders have actionable evidence of how state-of-the-art treatments alter functional trajectories after stroke.
Recent randomized trials have expanded the indications for both intravenous and intra-arterial therapies, optimizing procedural techniques and improving patient selection. Bridging thrombolysis, which combines tenecteplase with thrombectomy, has shown improved outcomes compared to thrombectomy alone, as demonstrated in large clinical trials.
Acute Treatments: Thrombectomy, Thrombolysis
Acute treatments must be administered within a narrow time window—typically within 4.5 hours for thrombolysis and up to 24 hours for thrombectomy in select cases. I always emphasize the importance of rapid hospital arrival and immediate imaging to determine eligibility for these interventions.
Emerging Therapies (RIC, VNS, etc.)
Emerging therapies such as remote ischemic conditioning (RIC) are being studied for their potential to enhance recovery in stroke patients. VNS has demonstrated benefits in improving motor function after stroke, while RIC may offer neuroprotection in acute settings. In my role as a physiatrist, I am closely following these developments to ensure I can offer the most up-to-date, evidence-based recommendations to both my clinical and legal clients.
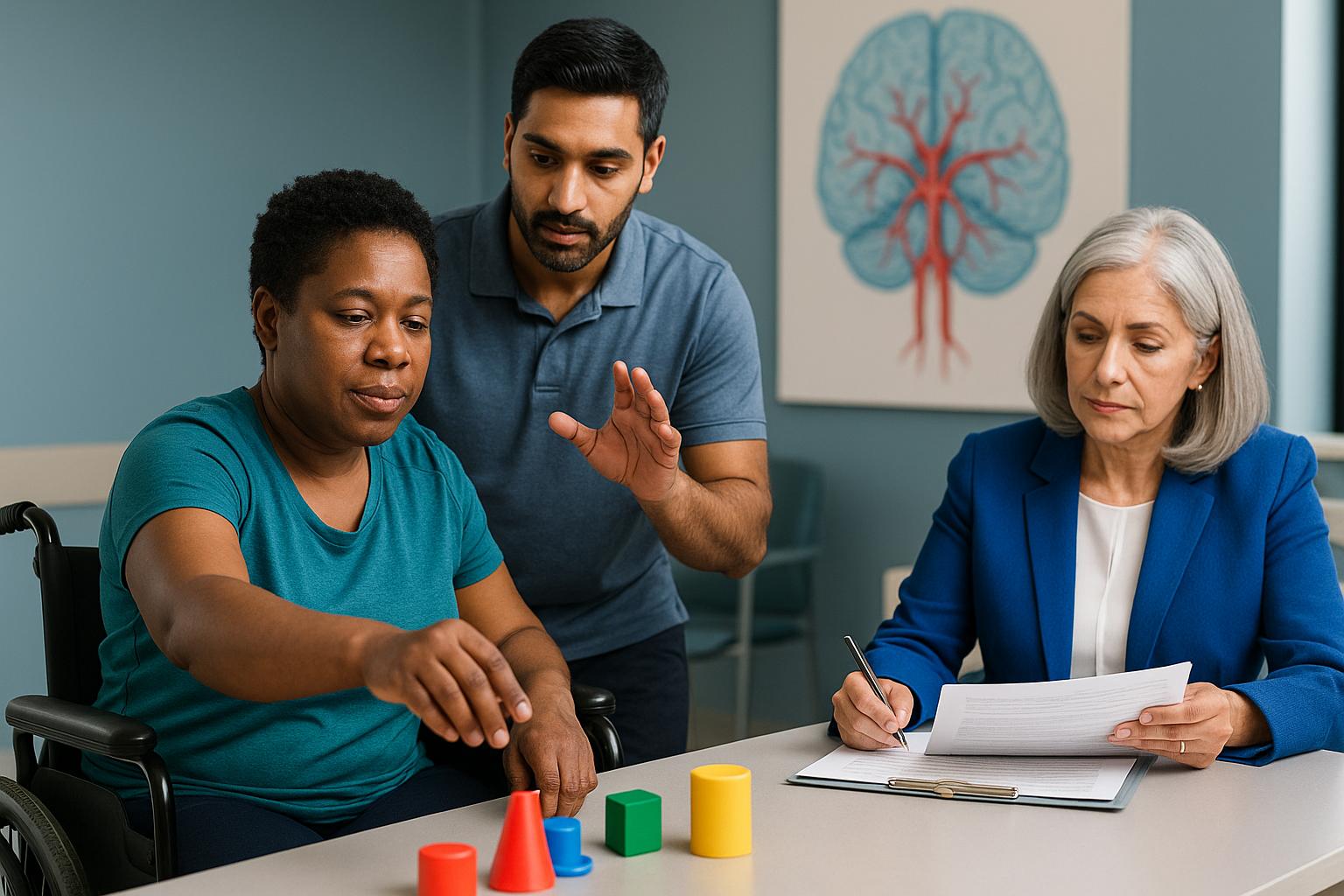
Rehabilitation After Ischemic Stroke
Rehabilitation is a cornerstone of recovery after ischemic stroke. Early, structured rehabilitation can improve activities of daily living and reduce long-term complications. In my experience as a triple board-certified physiatrist, I have observed that individualized rehabilitation plans yield the best outcomes. In fact, integrating my understanding of both neurorehabilitation and medico-legal principles, I am able to support optimal recovery pathways and provide objective evidence when impairment or disability is contested in a legal context.
Meta-analyses confirm that very early rehabilitation improves function, but caution is warranted—overly intense therapy in the acute phase may increase risk. Guidelines recommend balancing early intervention with patient safety.
Early Rehabilitation: Pros and Cons
Early rehabilitation can accelerate recovery, but must be tailored to the patient’s medical stability. I carefully assess each case to determine the optimal timing and intensity of therapy.
Long-Term Recovery Support
Long-term support may include physical, occupational, and speech therapy, as well as psychological counseling. I have found that ongoing follow-up and adjustment of the rehabilitation plan are essential for sustained improvement.
Telemedicine and Multi-State Expertise
Telemedicine has transformed access to stroke care, enabling rapid evaluation and specialist consultation across state lines. As a physician licensed in over 10 states, I provide both clinical and medico-legal expertise to a broad range of clients. Recent clinical trials demonstrate that telemedicine expands access to advanced treatments and improves outcomes, particularly in underserved areas.
My dual qualification as a DO and JD allows me to bridge the gap between medical and legal needs, offering objective analysis for both clinical management and damage assessment in litigation. I am committed to providing clear, accessible explanations of complex medical concepts for all parties involved.
From my perspective, this blended expertise positions me to communicate effectively with both treating physicians and attorneys, clarifying the nuances of functional recovery, impairment, and prognosis following ischemia and stroke, regardless of where a litigant resides or seeks care.
My Approach to Patient Care
Delivering care for individuals facing ischemia and stroke requires a commitment to both clinical precision and compassionate support. My philosophy is rooted in the belief that every patient deserves a thorough, evidence-based evaluation, whether the context is acute treatment, rehabilitation, or medico-legal assessment.
As a triple board-certified physician with dual degrees in medicine and law, I integrate the latest research with a nuanced understanding of functional outcomes and legal implications. My practice emphasizes clear communication, individualized care plans, and meticulous documentation—elements that are essential for both optimal recovery and fair legal adjudication.
I remain actively engaged in ongoing professional development, including participation in national conferences and review of emerging clinical trials. This ensures that my recommendations reflect the most current standards in both medical and legal practice.
Ultimately, my goal is to empower patients, families, and legal professionals with actionable information and expert guidance, supporting the best possible outcomes in every case of ischemia and stroke.
Ischemia and Stroke Expertise in Reno
As a physician based in Reno, I recognize the unique healthcare landscape of Northern Nevada and the surrounding region. In Nevada, approximately 12.4% of the population has diabetes, highlighting the importance of timely stroke prevention and intervention.
My Reno-based practice serves as a central resource for both medical and legal consulting, offering medical assessment and legal applications through specialized medical-legal services, including expert witness and independent medical evaluation services to local attorneys, claims professionals, and litigants. This ensures that complex cases receive objective, evidence-based analysis.
Telemedicine capabilities allow me to extend these services across Nevada and into additional licensed states, including Texas, California, Colorado, and beyond. This approach bridges gaps in access for rural and underserved communities, while maintaining a strong local presence in Reno.
If you are a patient, physician, attorney, or claims professional in Reno seeking advanced expertise in ischemia and stroke, I invite you to schedule a virtual second opinion or request a consultation tailored to your needs.
Conclusion
Ischemia and stroke represent a sudden, critical loss of blood flow to brain tissue, often resulting in rapid neurological injury and long-term disability. In summary, timely recognition, immediate intervention, and comprehensive documentation are essential for optimizing both medical recovery and legal outcomes.
As a triple board-certified physician and attorney, I understand the insurmountable importance of precise clinical management and objective legal analysis in every case. Recent advances—such as remote ischemic conditioning and early rehabilitation—offer new hope for improved function, while meticulous documentation supports fair adjudication of damages. For those facing complex questions about ischemia and stroke, my dual expertise ensures that both health and legal interests are protected.
Based in Reno, I provide specialized services across multiple states, including Texas, California, and Colorado, and others through both telemedicine and in-person consultations. I am willing to travel as an expert witness when needed, ensuring that patients and litigants with complex cases receive the highest standard of care and analysis, regardless of location.
I invite you to schedule a consultation TODAY to maximize your recovery outcomes and secure the thorough legal documentation you need. Working with a dual-qualified physician-attorney means you benefit from both advanced medical insight and precise legal clarity—prompt action can make all the difference for your health, your case, and your peace of mind.
This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
Frequently Asked Questions
What is the difference between ischemia and stroke?
Ischemia refers to a reduction or blockage of blood flow to brain tissue, depriving cells of oxygen and nutrients. When this process is severe or prolonged, it leads to a stroke—specifically, an ischemic stroke, which is the most common type. Recognizing this distinction is crucial for both timely treatment and accurate legal documentation.
How can I access your ischemia and stroke expertise regardless of my location?
You can access my expertise through telemedicine consultations across all states where I am licensed, including Texas, California, and Colorado. I also offer in-person evaluations and am willing to travel for complex cases or expert witness needs. This multi-state approach ensures that patients and legal professionals receive specialized care and analysis wherever they are.
How does your combined medical and legal expertise benefit those affected by ischemia and stroke?
My dual qualifications as a physician and attorney allow me to provide comprehensive assessments that address both medical recovery and legal documentation. This means I can objectively evaluate functional impairments, clarify causation, and support fair damage assessment—benefiting both plaintiffs and defendants in litigation, as well as treating physicians seeking clear, actionable reports.
About the Author
Dr. Ellia Ciammaichella, DO, JD, is a triple board-certified physician specializing in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine. With dual degrees in medicine and law, she offers a rare, multidisciplinary perspective that bridges clinical care and medico-legal expertise. Dr. Ciammaichella helps individuals recover from spinal cord injuries, traumatic brain injuries, and strokes—supporting not just physical rehabilitation but also the emotional and cognitive challenges of life after neurological trauma. As a respected independent medical examiner (IME) and expert witness, she is known for thorough, ethical evaluations and clear, courtroom-ready testimony. Through her writing, she advocates for patient-centered care, disability equity, and informed decision-making in both medical and legal settings.