What Is ISC Stroke? A Medical Guide to Ischemic Stroke Diagnosis and Care
By Dr. Ellia Ciammaichella, DO, JD — Triple Board-Certified in PM&R, SCI, and Brain Injury Medicine
Quick Insights
An ISC stroke, or ischemic stroke, is a sudden blockage of blood flow to the brain—usually from a blood clot—leading to brain cell damage. Common causes include high blood pressure and heart disease. Immediate expert care is critical, as lasting neurological and legal consequences often follow.
Key Takeaways
- ISC stroke makes up about 87% of all strokes, most often caused by blocked arteries in the brain.
- Symptoms often appear quickly: weakness, speech change, and vision loss signal urgent need for emergency attention.
- Recent guidelines stress sleep, diet, and activity as vital stroke prevention factors for everyone.
- Distinguishing ISC stroke from hemorrhagic or other CVA types shapes both treatment and rehabilitation options.
Why It Matters
Understanding ISC stroke empowers you to recognize emergencies, advocate for evidence-based treatment, and anticipate both health and legal implications for your family’s future. Immediate action and informed choices after a stroke can mean the difference between lifelong challenges and optimal recovery.
Introduction
As both a physician and attorney, I routinely encounter confusion surrounding the term “ISC stroke” and its profound personal and legal impact.
ISC stroke—also known as ischemic stroke or cerebral vascular accident (CVA)—is a sudden blockage of blood flow to the brain, usually caused by a clot, resulting in immediate brain tissue injury. This condition represents the vast majority of all strokes, requiring rapid diagnosis and intervention for optimal treatment outcomes and accurate medicolegal assessment.
My dual training in Physical Medicine and Rehabilitation (PM&R), Spinal Cord Injury Medicine, and Brain Injury Medicine allows me to address the intricate overlap between timely clinical care and the vital documentation necessary for insurance, legal review, or family advocacy.
For more information on my unique qualifications as both a physician (DO) and attorney (JD), please see my professional bio here. According to the latest AHA/ASA guidelines, prevention demands a multidisciplinary, holistic approach including sleep, diet, and blood pressure optimization.
For every patient, family, or professional in Reno or nationwide, understanding both the medical and legal facets of ISC stroke is essential—clarity empowers better outcomes and proactive decisions.
What is an ISC Stroke?
An ISC stroke, or ischemic stroke, is defined as a sudden interruption of blood flow to a region of the brain, most commonly due to an arterial blockage by a thrombus or embolus. This deprivation of oxygen and nutrients results in rapid neuronal injury and, if not promptly addressed, irreversible brain tissue loss. The term “ISC” is simply an abbreviation for “ischemic,” and is used interchangeably in clinical and legal documentation.
Understanding ‘ISC’ vs. ‘Ischemic’ Medical Terms
The distinction between “ISC” and “ischemic” is purely linguistic; both refer to the same pathophysiological process. In my practice, I have found that confusion often arises when medical records, insurance forms, or legal documents use these terms inconsistently.
For clarity, I always ensure that all parties—patients, families, and legal professionals—understand that “ISC stroke” and “ischemic stroke” are synonymous, both denoting a blockage-based cerebrovascular event.
Clear and consistent medical terminology can facilitate better communication between healthcare providers and may contribute to more accurate documentation in clinical settings. Standardized medical terminology is generally recognized as important for healthcare communication, though its specific impact on medicolegal outcomes requires further study.
Types of Stroke: Ischemic vs. Hemorrhagic
Strokes are broadly categorized into two principal types: ischemic and hemorrhagic. Ischemic strokes, including ISC strokes, account for the majority of cases and are caused by vascular occlusion. Hemorrhagic strokes, in contrast, result from rupture of a cerebral blood vessel, leading to bleeding within or around the brain.
Hemorrhagic Stroke Basics
Hemorrhagic strokes are less common but often more severe, involving either intracerebral or subarachnoid hemorrhage. The sudden release of blood increases intracranial pressure and can rapidly compromise neurological function. In my experience, distinguishing between ischemic and hemorrhagic stroke is critical, as the treatments are fundamentally different and misclassification can have dire consequences.
Other Stroke Types
Other, less common cerebrovascular events include transient ischemic attacks (TIAs), which are brief episodes of neurological dysfunction without permanent damage, and cerebral venous sinus thrombosis (CVST), which involves clotting in the brain’s venous system. Each type requires a tailored diagnostic and therapeutic approach, and I emphasize the importance of precise classification in both clinical and medicolegal settings.
Comprehensive functional assessment, beyond basic diagnosis, is commonly considered important in medicolegal evaluations of neurological injuries, though specific evidence supporting this practice varies. Documenting stroke subtype and specific impairment—for both medical and legal purposes—ensures every party understands the impact on daily living and long-term needs.
ISC Stroke vs. CVA: Clearing Up Confusion
The term “CVA” (cerebrovascular accident) is a broad descriptor encompassing all types of stroke, including both ischemic and hemorrhagic subtypes. However, in clinical and legal documentation, specificity is paramount.
Definitions Simplified
An ISC stroke is a specific type of CVA characterized by arterial blockage. In contrast, a CVA may refer to any sudden neurological deficit due to vascular causes, including hemorrhagic events. I routinely clarify these distinctions in my reports to ensure that all parties—medical, legal, and insurance—are aligned in their understanding.
Why Terminology Matters
Precise terminology is essential for accurate diagnosis, treatment planning, and legal documentation. In my dual role as a physician and legal consultant, I have observed that ambiguous language can lead to misinterpretation of medical records, affecting both patient care and the outcome of legal proceedings.
From my unique perspective with both medical and legal training, I can translate complex medical findings into precise documentation that clearly establishes functional limitations for both plaintiff and defense teams. While some medical experts focus solely on diagnosis, my approach emphasizes comprehensive functional assessment that provides all parties—physicians, attorneys, and litigants—with clear, accessible documentation of impairments.
For those needing a thorough evaluation that connects both medical assessment and legal applications—such as expert witness reports, independent medical examinations, or damage analysis—please explore my comprehensive medical-legal services for ISC stroke and other injuries.
Causes and Risk Factors of ISC Stroke
ISC strokes are most frequently caused by atherosclerosis, cardiac emboli, or small vessel disease. Major risk factors include hypertension, diabetes, hyperlipidemia, atrial fibrillation, and smoking. Recent research has also identified sleep disorders as a significant, modifiable risk factor.
Common Risk Factors
- High blood pressure
- Diabetes mellitus
- High cholesterol
- Smoking
- Atrial fibrillation
- Sleep apnea and poor sleep quality
I have seen that addressing these risk factors through lifestyle modification and medical management can substantially reduce stroke incidence. According to the 2024 AHA/ASA guidelines, a holistic approach—including sleep, diet, and physical activity—is now considered standard for primary prevention.
Based on treating hundreds of patients with ischemic and hemorrhagic strokes, I know that early, personalized risk assessment is not only vital for health but also directly influences how damages are evaluated in insurance and legal claims. Preventing a second event can be just as important as managing the aftermath of the first.
Prevention Insights
Preventive strategies must be individualized, accounting for each person’s unique risk profile. I advise both patients and litigants that comprehensive risk assessment and early intervention are crucial, not only for health but also for accurate damage assessment in legal contexts.
Symptoms and Diagnosis
ISC stroke symptoms typically develop suddenly and may include unilateral weakness, speech disturbances, vision loss, and facial droop. Rapid recognition and diagnosis are essential to minimize brain injury and optimize outcomes.
Key Warning Signs
- Sudden weakness or numbness, especially on one side
- Difficulty speaking or understanding speech
- Sudden vision changes
- Severe headache without a known cause
In my clinical experience, prompt identification of these signs by family members or bystanders is often the determining factor in a patient’s recovery trajectory.
How Stroke Is Diagnosed
Diagnosis relies on a combination of clinical assessment and neuroimaging, such as CT or MRI scans, to distinguish between ischemic and hemorrhagic stroke. Laboratory tests and cardiac evaluation may also be necessary to identify underlying causes. I emphasize the importance of immediate imaging, as treatment decisions hinge on accurate stroke type identification.
Thorough functional assessment and documentation are generally considered important components of medicolegal evaluations, though the relationship between assessment quality and legal outcomes varies by case. Initial diagnostic findings typically inform subsequent clinical assessments, though the relationship between early diagnosis and long-term functional outcomes can vary significantly.
When to Seek Medical Attention
Seek immediate medical attention if you or someone you know experiences sudden weakness, speech difficulty, or vision loss. Early intervention by a physician is critical to reducing the risk of permanent disability.
Acute Treatment and New Research
Acute management of ISC stroke centers on restoring cerebral blood flow as quickly as possible. Intravenous thrombolysis with tissue plasminogen activator (tPA) and mechanical thrombectomy are the mainstays of therapy, with time-to-treatment being the most critical determinant of outcome.
Recent advances presented at the International Stroke Conference have expanded the therapeutic window for certain interventions and introduced novel agents, such as intra-arterial tenecteplase, which can be administered during thrombectomy up to 24 hours after symptom onset. This approach has demonstrated improved outcomes in select patients, as highlighted in ISC 2025 conference coverage.
I have observed that integrating these new protocols into practice requires close coordination among emergency, neurology, and interventional teams. Additionally, individualized treatment approaches based on patient characteristics and diagnostic findings are widely discussed in clinical literature, though specific evidence supporting optimal selection criteria continues to evolve.
Landmark randomized controlled trials, such as MR CLEAN and ESCAPE, have fundamentally changed the standard of care for acute ischemic stroke, as summarized in systematic reviews. Ongoing research continues to refine these approaches, with adaptive trial designs and modern data infrastructure improving inclusivity and efficiency in global stroke research.
From my vantage point as a dual-degreed DO and JD, I remain vigilant about how the latest treatment protocols and outcome metrics affect not only patient recovery but also the medicolegal estimation of disability and prognostic value for legal claims. Staying abreast of these research evolutions is a core responsibility I bring to both my clinical and medical-legal consulting work.
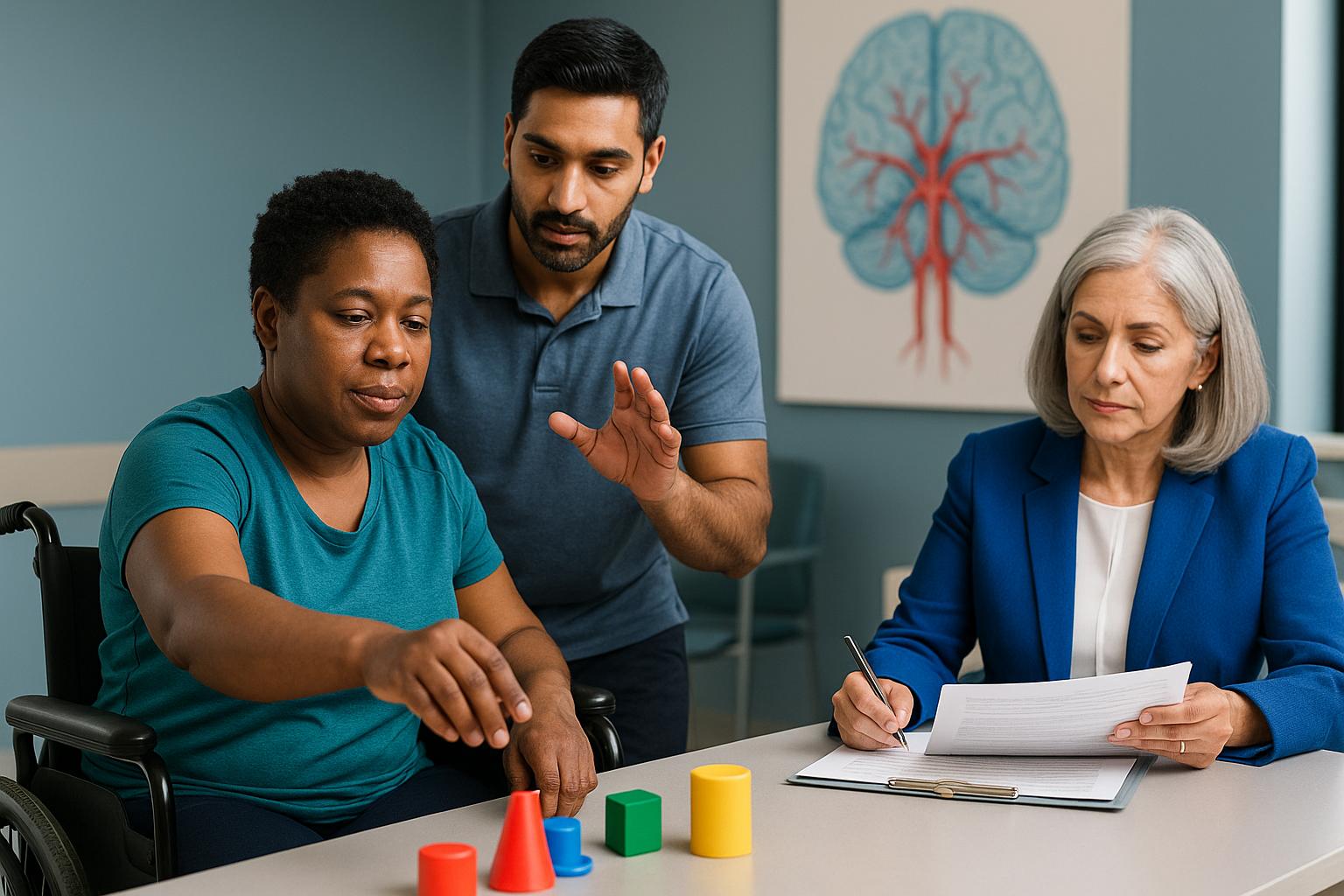
Stroke Recovery and Rehabilitation
Recovery from ISC stroke is a dynamic process, influenced by the extent of brain injury, patient comorbidities, and the timing and intensity of rehabilitation. Early initiation of rehabilitation has been shown to improve functional outcomes and reduce long-term disability.
Intensive inpatient rehabilitation, particularly in specialized facilities, is associated with better recovery compared to less intensive settings, as demonstrated in policy statements and systematic reviews. In my practice, I prioritize early mobilization and multidisciplinary therapy, which aligns with the latest evidence.
Ongoing clinical trials, such as those coordinated by major academic centers, are evaluating new rehabilitation strategies and technologies to further enhance recovery. I encourage both patients and legal professionals to consider the full spectrum of rehabilitation options when assessing prognosis and damages.
Extensive experience in clinical settings indicates that functional recovery after ISC stroke can differ greatly depending on early rehab access and coordinated discharge planning. My analysis of damages—whether for plaintiffs or defendants—always accounts for the potential gains achieved through intensive rehabilitation and the substantial evidence base supporting these approaches.
The complex intersection between medical progress and legal outcomes is one reason I have devoted my career to bridging clinical assessment with expert witness consultation for stroke-related cases.
My Approach to Patient Care and Expertise
Delivering clarity and confidence to individuals and families facing an ISC stroke is central to my practice philosophy. My dual training as a physician and attorney allows me to bridge the gap between complex medical concepts and the legal realities that often follow a cerebrovascular event.
I am triple board-certified in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine. This unique combination enables me to provide not only evidence-based clinical care but also precise, accessible documentation for insurance, legal, and advocacy purposes. I remain actively engaged with the latest research and national guidelines, ensuring that every assessment and recommendation is grounded in current best practices.
In my Reno-based practice, I emphasize individualized care, thorough functional assessment, and transparent communication. Whether I am supporting a patient’s rehabilitation or providing expert witness analysis for a litigant, my goal is to empower informed decisions and optimal outcomes.
If you or your family are navigating the aftermath of an ISC stroke, I encourage you to seek a second opinion or consultation. My expertise is available both locally and via telemedicine across multiple states, ensuring access to specialized guidance wherever you are.
ISC Stroke Assessment and Legal Consulting in Reno
Reno serves as the primary hub for my ISC stroke assessment and consulting services, offering both in-person and telemedicine options for patients, physicians, attorneys, and claims professionals. The unique demographic and healthcare landscape in Reno, including a mix of urban and rural populations, often influences both the presentation and management of cerebrovascular events.
As a physician based in Reno with licensure across Texas, California, and several other states, I am able to address the needs of local residents while also providing expert witness and damage assessment services for legal cases throughout the region. My practice is distinguished by its integration of medical and legal expertise, supporting both acute care and the complex documentation required for litigation or insurance claims.
Local physicians, attorneys, and litigants in Reno benefit from my ability to deliver comprehensive, evidence-based evaluations that meet the highest standards for both clinical and legal accuracy. Telemedicine extends these services to those in outlying areas, ensuring that geographic barriers do not impede access to specialized stroke care or expert analysis.
If you are in Reno or the surrounding region and require ISC stroke assessment, rehabilitation planning, or medicolegal consultation, I invite you to connect with my practice. Schedule a virtual second opinion or request an IME consultation to ensure your case receives the attention and expertise it deserves.
Conclusion
An ISC stroke, or ischemic stroke, is a sudden blockage of blood flow to the brain, most often caused by a clot, resulting in immediate neurological injury and complex medical-legal implications. In summary, timely recognition and intervention are essential for optimal recovery, while precise documentation is critical for legal clarity and fair damage assessment.
My dual qualifications as a triple board-certified physician and attorney uniquely position me to address both the clinical and legal dimensions of ISC stroke, ensuring that every patient and litigant receives comprehensive, evidence-based guidance.
Based in Reno, I provide specialized services across multiple states, including Texas, California, and Colorado, through both telemedicine and in-person consultations. I am willing to travel as an expert witness, offering flexibility that benefits individuals and professionals managing complex stroke cases.
If you are seeking clarity about your stroke case, I invite you to schedule a consultation TODAY to secure the best possible recovery outcomes and ensure your legal documentation is thorough and defensible. Prompt action can make a significant difference in both health and legal peace of mind during challenging times.
This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
Frequently Asked Questions
What is an ISC stroke, and how is it different from a CVA?
An ISC stroke, or ischemic stroke, is a type of cerebrovascular accident (CVA) caused by a blocked artery in the brain, leading to reduced blood flow and brain cell damage. While all ISC strokes are CVAs, not all CVAs are ischemic—some are hemorrhagic, caused by bleeding rather than blockage. Accurate classification is crucial for both treatment and legal documentation.
How can I access your ISC stroke expertise regardless of my location?
You can access my ISC stroke expertise through telemedicine consultations in all states where I am licensed, including Texas, California, and Colorado. I also offer in-person assessments and am willing to travel for complex cases or expert witness needs. This multi-state approach ensures that patients and professionals receive specialized care and analysis wherever they are.
How does your combined medical and legal expertise benefit ISC stroke cases?
My dual training as a physician and attorney allows me to provide both evidence-based medical care and precise legal documentation. This ensures that every aspect of an ISC stroke—clinical management, functional assessment, and damage evaluation—is addressed thoroughly, supporting fair outcomes for both plaintiffs and defendants in legal proceedings.
About the Author
Dr. Ellia Ciammaichella, DO, JD, is a triple board-certified physician specializing in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine. With dual degrees in medicine and law, she offers a rare, multidisciplinary perspective that bridges clinical care and medico-legal expertise. Dr. Ciammaichella helps individuals recover from spinal cord injuries, traumatic brain injuries, and strokes—supporting not just physical rehabilitation but also the emotional and cognitive challenges of life after neurological trauma. As a respected independent medical examiner (IME) and expert witness, she is known for thorough, ethical evaluations and clear, courtroom-ready testimony. Through her writing, she advocates for patient-centered care, disability equity, and informed decision-making in both medical and legal settings.