Stroke Rehabilitation Breakthrough: Milestones That Restore Hope
By Ellia Ciammaichella, DO, JD
Triple Board-Certified in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine
Quick Insights
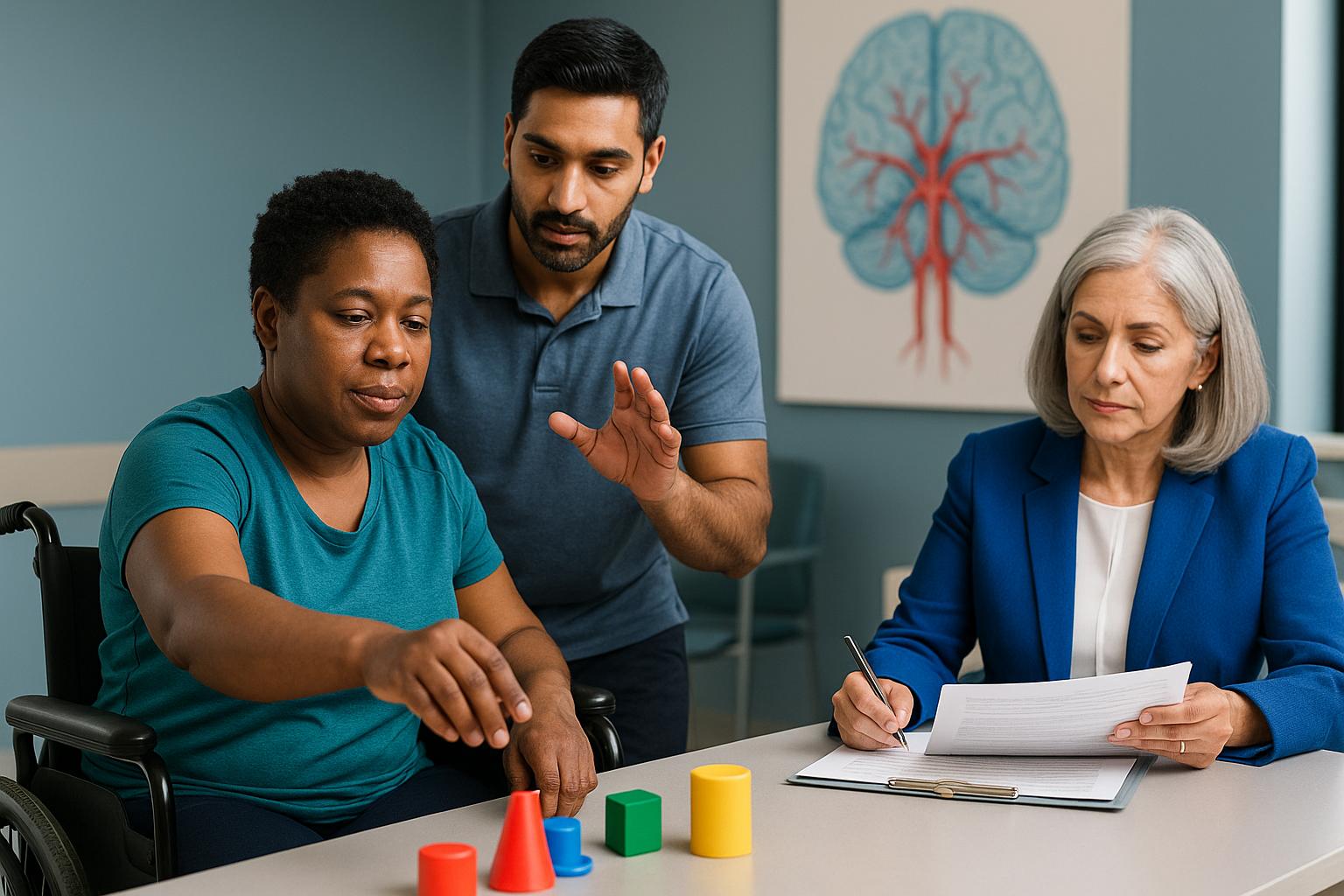
Stroke rehabilitation is a structured, time-sensitive process that follows predictable phases to restore lost function. Recovery involves coordinated care from multiple specialists targeting motor skills, mobility, and daily activities.
Key Takeaways
- Organized, interprofessional rehabilitation care improves outcomes more than fragmented approaches across all stroke severities.
- Robot-assisted gait training added to conventional therapy enhances balance and walking ability in subacute phases.
- Mirror therapy for upper limb recovery shows dose-dependent effects, with more frequent sessions yielding greater hand function.
- Very early rehabilitation within 48 hours may improve motor outcomes but requires careful medical monitoring.
Why It Matters
Understanding realistic recovery timelines helps families plan care and attorneys evaluate whether rehabilitation met accepted standards. Knowing which milestones typically occur in each phase clarifies whether delays or gaps in therapy affected long-term function. This knowledge supports informed decisions about ongoing care needs and functional prognosis.
Introduction
As a board-certified physician and attorney, I evaluate stroke cases where recovery expectations and rehabilitation adequacy are disputed. My comprehensive background enables me to provide nuanced, evidence-based analysis—learn more about Ellia Ciammaichella, DO, JD and my medical and legal expertise.
Stroke rehabilitation is a structured, time-sensitive process designed to restore lost motor, cognitive, and functional abilities after brain injury. Organized, coordinated interprofessional care improves outcomes across all stroke severities compared to fragmented approaches. Most functional gains occur within the first 12 weeks, with continued improvement through 24 weeks, though timing and intensity of therapy significantly influence results.
Understanding realistic recovery timelines helps attorneys evaluate whether rehabilitation met accepted standards. Knowing which milestones typically occur in each phase clarifies whether delays or gaps in therapy affected long-term function.
This article outlines evidence-based recovery phases, functional goals, and realistic timelines grounded in clinical guidelines and recent research.
Understanding Stroke Rehabilitation Phases
Stroke rehabilitation follows a structured timeline divided into distinct phases, each with specific goals and intensity requirements. The acute phase of stroke rehabilitation begins immediately after onset and typically lasts up to 7 days, emphasizing medical stabilization and early mobilization. During this period, medical stability takes priority, but rehabilitation dosage and multidisciplinary team coordination begin shaping early recovery trajectories.
The subacute phase begins within the first week post-stroke and continues up to six months, featuring intensive efforts to promote neurological recovery and enhance function. This window represents the period of most rapid functional gains. Rehabilitation intensity during subacute recovery typically involves 3 hours of therapy daily, distributed across physical, occupational, and speech therapy disciplines. The chronic phase begins at six months post-stroke, with recovery progress slowing, but targeted interventions can help maintain gains and prevent decline.
In my medical-legal evaluations, I often see disputes centered on whether rehabilitation intensity met guideline standards during the subacute phase. Understanding these phase-specific expectations helps clarify whether care delivery aligned with accepted protocols or whether gaps in therapy timing or coordination may have limited functional outcomes.
Early Recovery Milestones: The First 12 Weeks
Most functional gains occur within the first 12 weeks after stroke, with continued but slower improvement through 24 weeks. This empirical timeline establishes realistic expectations for motor recovery, activities of daily living, and mobility restoration. Early milestones include regaining sitting balance, initiating voluntary movement in affected limbs, and beginning transfers with assistance.
Timing of rehabilitation initiation significantly influences outcomes. Very early rehabilitation within 48 hours can improve motor function and activities of daily living, though medical stability must be carefully monitored. Premature mobilization in unstable patients carries risks, requiring physician oversight to balance intensity with safety.
Self-care progresses from basic activities, such as feeding and grooming, to more complex tasks like dressing and bathing, with timelines varying based on individual recovery. Mobility goals advance from bed mobility to standing, then to walking with assistive devices. When reviewing medical records in these cases, I focus on whether therapy documentation reflects progression through these expected milestones or whether recovery plateaued prematurely due to inadequate intervention frequency.
Motor Function Recovery and Upper Limb Milestones
Upper limb recovery follows a predictable but variable pattern, with hand function often lagging behind proximal arm movement. Initial motor return typically appears in shoulder and elbow muscles before progressing distally to wrist and finger control. Functional milestones include reaching for objects, grasping and releasing items, and eventually performing fine motor tasks like buttoning or writing.
Mirror therapy demonstrates dose-dependent effects on upper limb function, with more frequent sessions yielding greater improvements in hand function. This intervention uses visual feedback from the unaffected limb to stimulate motor cortex reorganization in the affected hemisphere. The evidence supports incorporating mirror therapy as an adjunct to conventional therapy, particularly for patients with moderate upper limb impairment.
Recovery potential varies significantly based on initial stroke severity and lesion location. Patients with complete paralysis at onset face different trajectories than those with partial weakness. In medical-legal evaluations, I look closely at baseline assessments and whether therapy plans appropriately matched the patient’s recovery potential and functional goals.
Gait and Mobility Recovery Timelines
Walking recovery represents a primary rehabilitation goal for most stroke survivors. Early gait milestones include standing tolerance, weight shifting between legs, and taking initial steps with maximum assistance. Progression continues through walking with assistive devices, advancing from parallel bars to walkers, then to canes or independent ambulation.
Robot-assisted gait training added to conventional therapy improves balance and walking ability, particularly during subacute phases. These devices provide body weight support and guided leg movement, allowing higher-intensity practice than manual assistance alone. Evidence shows greater gains when robot-assisted training begins in subacute stages rather than chronic phases.
Balance recovery parallels gait progression but requires specific attention. Patients must regain sitting balance before standing, and standing balance before walking. Falls during rehabilitation can delay progress and cause additional injuries. When evaluating whether rehabilitation met standards, I consider whether balance training received adequate emphasis alongside mobility practice.
For additional perspective on complex recovery pathways beyond stroke rehabilitation—such as how recovery milestones are evaluated after spinal cord injury—see this detailed guide on signs of improvement in spinal cord injury recovery.
Technology-Enhanced Rehabilitation Approaches
Advanced rehabilitation technologies offer mechanisms to augment traditional therapy approaches. Virtual reality-inclusive rehabilitation improves functional outcomes through augmented sensorimotor feedback that enhances motor learning. These systems provide repetitive, task-specific practice in engaging formats that may increase therapy tolerance and intensity.
Robot-assisted devices for both upper and lower limbs allow higher repetition counts than manual therapy alone. The technology provides consistent, measurable assistance that can be gradually reduced as patients improve. However, technology does not replace skilled therapist judgment about exercise selection, progression, and functional application.
In my practice evaluating rehabilitation adequacy, I assess whether technology use aligned with evidence-based indications and whether it supplemented rather than replaced conventional therapy. Technology-enhanced approaches work best when integrated into comprehensive programs that address multiple recovery domains simultaneously.
To understand the breadth of objective medical-legal consulting services available—including expert witness testimony and IMEs supporting stroke rehabilitation cases—review the expertise offered by Ciammaichella Consulting Services, PLLC.
Long-Term Functional Recovery Expectations
Beyond six months post-stroke, recovery may continue at a slower pace, potentially involving improvements in abilities already regained, such as increased walking speed and hand dexterity; however, some stroke survivors may experience lasting impairments requiring ongoing adaptation. Chronic-phase gains typically involve refinement of existing abilities rather than emergence of entirely new functions. Patients who achieve independent walking by 6 months may continue improving speed and endurance. Those who regain basic hand function may develop better dexterity and coordination.
Realistic long-term expectations depend on multiple factors including stroke severity, lesion location, age, and comorbidities. Complete recovery occurs in only a minority of stroke survivors. Most patients retain some degree of permanent impairment requiring ongoing adaptation strategies and assistive devices.
From a medical-legal perspective, understanding these long-term trajectories helps distinguish between expected residual deficits and outcomes potentially influenced by rehabilitation inadequacies. Permanent functional limitations do not necessarily indicate substandard care, but failure to achieve expected milestones during optimal recovery windows may warrant scrutiny of therapy intensity, duration, and coordination.
How I Support Attorneys in Stroke Rehabilitation Cases
In my medical-legal evaluations, I often encounter disputes about whether stroke rehabilitation met accepted standards or whether gaps in therapy timing affected long-term outcomes.
With both medical and legal training, I can translate complex rehabilitation findings into precise documentation that clearly establishes functional limitations for both plaintiff and defense teams. From my unique perspective with dual credentials, I assess whether therapy intensity, duration, and coordination aligned with AHA/ASA guidelines during critical recovery windows.
Having evaluated hundreds of stroke cases, I’ve found that accurate functional assessment and milestone documentation are equally valuable for plaintiffs seeking fair compensation and defendants requiring objective analysis. My approach emphasizes comprehensive evaluation of rehabilitation adequacy—examining whether therapy dosage met standards, whether progression through expected milestones occurred appropriately, and whether any delays potentially influenced functional outcomes.
Individual case outcomes vary based on stroke severity, lesion location, and patient-specific factors.
Conclusion
In summary, stroke rehabilitation follows predictable phases with most functional gains occurring in the first 12 weeks. Understanding these timelines helps clarify whether therapy intensity and coordination met accepted standards during critical recovery windows. Robot-assisted training and other technology-enhanced approaches offer adjunctive benefits but do not replace comprehensive, multidisciplinary care that addresses motor, cognitive, and functional domains simultaneously.
As a physician and attorney, I evaluate whether rehabilitation programs delivered appropriate intensity, duration, and coordination aligned with AHA/ASA guidelines. My dual training allows me to translate complex rehabilitation findings into precise documentation that establishes functional limitations and recovery trajectories for both plaintiff and defense teams.
Through Ciammaichella Consulting Services, PLLC, based in Reno, Nevada, I provide medical-legal services across licensed states such as Texas, California, and Colorado. I am available to travel for expert testimony and in-person evaluations when appropriate. This flexibility allows individuals and legal teams with complex cases to access consistent, expert analysis regardless of location.
I invite you to request a consultation today to discuss how accurate functional assessment and milestone documentation can support your stroke rehabilitation case, whether you need objective analysis of therapy adequacy or expert testimony on expected recovery trajectories.
This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
Frequently Asked Questions
What is the typical timeline for regaining walking ability after stroke?
Most patients who will regain independent walking do so within the first 12 weeks after stroke, with continued refinement through 24 weeks. Initial milestones include standing tolerance and weight shifting, progressing to assisted walking with devices, then advancing to independent ambulation. Robot-assisted gait training combined with conventional therapy can accelerate balance and mobility gains, particularly when initiated during subacute phases. Recovery potential varies significantly based on stroke severity, lesion location, and rehabilitation intensity during optimal recovery windows.
How does early rehabilitation timing affect functional outcomes?
Very early rehabilitation initiated within 48 hours after stroke can improve motor function and activities of daily living, though medical stability must be carefully monitored. The first 12 weeks represent the period of most rapid functional gains, making therapy intensity and coordination during this window critical to long-term outcomes. Delays in initiating appropriate rehabilitation or gaps in therapy frequency during subacute phases may limit functional recovery potential and milestone achievement.
What role does technology play in stroke rehabilitation milestones?
Technology-enhanced approaches like virtual reality and robot-assisted training provide mechanisms for higher-intensity, repetitive practice that may augment traditional therapy. These modalities work best when integrated into comprehensive programs addressing multiple recovery domains simultaneously. However, technology does not replace skilled therapist judgment about exercise selection, progression, and functional application. Evidence shows technology-enhanced rehabilitation improves specific outcomes when used appropriately during subacute phases, though realistic expectations must account for stroke severity and baseline function.
About the Author
Dr. Ellia Ciammaichella, DO, JD, is a triple board-certified physician specializing in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine. With dual degrees in medicine and law, she offers a rare, multidisciplinary perspective that bridges clinical care and medico-legal expertise. Dr. Ciammaichella helps individuals recover from spinal cord injuries, traumatic brain injuries, and strokes—supporting not just physical rehabilitation but also the emotional and cognitive challenges of life after neurological trauma. As a respected independent medical examiner (IME) and expert witness, she is known for thorough, ethical evaluations and clear, courtroom-ready testimony. Through her writing, she advocates for patient-centered care, disability equity, and informed decision-making in both medical and legal settings.