AICA Stroke Symptoms? A Physician-Led, Evidence-Based Overview
By Dr. Ellia Ciammaichella, DO, JD — Triple Board-Certified in PM&R, Spinal Cord Injury Medicine, and Brain Injury Medicine
Quick Insights
AICA stroke symptoms refer to neurological problems caused by blockage in the anterior inferior cerebellar artery (AICA), triggering sudden vertigo, hearing loss, facial weakness, and balance changes. Immediate recognition is crucial for both patient outcome and legal clarity.
Key Takeaways
- AICA stroke often presents with vertigo, unilateral hearing loss, and facial paralysis.
- This type of stroke is rare, representing just 3% of all ischemic strokes.
- Symptoms can mimic conditions like Meniere’s disease but signal serious brain circulation loss.
- Prompt identification affects both medical recovery and accurate legal documentation for impacted cases.
Why It Matters
Recognizing AICA stroke symptoms quickly can save lives and ensure proper rehabilitation, while clear documentation helps resolve future legal questions. If left unaddressed, patients and legal professionals may face preventable harm or confusion over often-misunderstood neurological findings.
Introduction
As both a Doctor of Osteopathic Medicine and a Juris Doctor, I recognize how often AICA stroke symptoms generate confusion not only in clinical settings but also within legal proceedings. For more about my unique qualifications spanning both medical and legal fields, see my DO/JD professional biography.
AICA stroke symptoms are the neurological disturbances that result from diminished blood flow within the anterior inferior cerebellar artery—a vessel supplying critical regions of the brainstem and inner ear. These symptoms typically manifest as acute vertigo, unilateral hearing loss, facial paralysis, and dramatic balance impairment.
Understanding what is an AICA stroke, medically termed “anterior inferior cerebellar artery infarction,” matters profoundly because these presentations may closely mimic other disorders yet portend a serious underlying vascular event whose timely identification impacts both patient outcomes and medicolegal clarity.
In my dual capacity, I have seen firsthand that early, accurate recognition and documentation of these rare symptoms can influence both the trajectory of medical recovery and the defensibility of later legal assessments.
Research demonstrates that posterior circulation infarcts account for about 20% of ischemic strokes, with cerebellar infarcts— including AICA territory strokes—representing only 3% of all ischemic strokes, underscoring the rarity and complexity of such cases.
Clear, objective identification of AICA stroke symptoms supports not only optimal treatment in specialized centers but also establishes the foundational record for thorough legal evaluation when needed.
What Is an AICA Stroke?
An Anterior Inferior Cerebellar Artery (AICA) stroke is a rare type of ischemic stroke that occurs when blood flow is obstructed in the AICA, a vessel supplying the lower lateral pons, inner ear, and parts of the cerebellum.
This vascular event leads to a constellation of neurological deficits that are both distinctive and diagnostically challenging. In my experience, the rarity of AICA strokes—comprising only about 3% of all ischemic strokes—often results in delayed recognition, particularly when symptoms overlap with more common conditions such as vestibular neuritis or Meniere’s disease.
The AICA’s anatomical territory includes structures responsible for balance, hearing, and facial movement. When this artery is compromised, the resulting infarction can produce a combination of vertigo, unilateral hearing loss, facial weakness, and ataxia. These symptoms are not only sudden in onset but also frequently misattributed to benign inner ear disorders, which can complicate both acute management and subsequent legal evaluation.
I have found that a precise understanding of the vascular anatomy and its clinical implications is essential for both accurate diagnosis and effective communication in medicolegal contexts.
AICA strokes are particularly insidious because their initial presentation may be subtle or incomplete. For example, a litigant may present with isolated vertigo or hearing loss, only to develop more severe deficits over hours or days.
This evolving symptomatology underscores the importance of early, comprehensive neurological assessment and documentation. According to current clinical guidance, the overlap with other posterior circulation strokes further complicates the diagnostic process, making expert evaluation indispensable.
Key Symptoms of AICA Stroke
AICA stroke symptoms are best understood as a spectrum, ranging from classic, well-recognized features to atypical or overlapping presentations. In my dual role as a physician and legal consultant, I have seen how the nuanced presentation of these symptoms can impact both clinical outcomes and the clarity of medicolegal reports.
Core AICA stroke symptoms include:
- Sudden vertigo (spinning sensation)
- Unilateral hearing loss (typically on the same side as the stroke)
- Facial weakness or paralysis
- Ataxia (loss of coordination or balance)
- Nausea and vomiting
- Nystagmus (involuntary eye movements)
- Tinnitus (ringing in the ears)
These symptoms often appear abruptly and may progress over several hours. In my practice, I have observed that the combination of vertigo and hearing loss is particularly suggestive of AICA involvement, especially when accompanied by facial weakness. Research confirms that vertigo and unilateral deafness are hallmark features, with larger strokes producing more pronounced facial paralysis and ataxia.
Classic/Core Symptoms
The classic presentation involves:
- Acute vertigo that is severe and persistent
- Ipsilateral (same side) hearing loss or tinnitus
- Facial paralysis or numbness
- Gait instability and limb incoordination
These findings are highly specific for AICA territory infarction. I have found that prompt recognition of this triad—vertigo, hearing loss, and facial weakness—can expedite both neuroimaging and intervention, improving patient outcomes. Facial droop, in particular, is due to involvement of the facial nuclei rather than the nerve itself, distinguishing it from other pontine syndromes as detailed in clinical guidance.
In my 15+ years of practice evaluating individuals with spinal cord and brain injuries, I’ve found that detailed functional assessment, beyond basic diagnosis, is essential for accurately delineating damages in legal proceedings. When a litigant presents with this classic triad, I make it a priority to meticulously document initial findings, since evolving symptoms may later complicate both medical management and objective injury valuation.
Atypical or Overlapping Symptoms
AICA strokes may also present with:
- Symptoms mimicking Meniere’s disease (fluctuating hearing, tinnitus, episodic vertigo)
- Isolated auditory or vestibular loss without other brainstem signs
- Bilateral hearing fluctuation (rare, but suggests vascular etiology)
- Headache, vomiting, or neck stiffness
In my experience, these atypical features can delay diagnosis, especially when initial symptoms are attributed to benign inner ear disorders. Some cases may even mimic Bell’s palsy, with facial weakness predominating. Recent research highlights that bilateral symptoms or diagnostic uncertainty should prompt urgent vascular evaluation.
From my perspective as a triple board-certified physiatrist with both medical and legal training, I recognize how easy it is for these atypical symptoms to be dismissed. I often advise both medical colleagues and attorneys to consider vascular causes even when presentations deviate from textbook cases, as overlooking early subtle signs can result in significant functional impairment or missed legal damages.
When to Seek Medical Attention
Seek immediate evaluation by a physician if you or your client experience:
- Sudden, severe vertigo with hearing loss
- New facial weakness or paralysis
- Loss of balance or inability to walk
How Is an AICA Stroke Diagnosed?
Diagnosing an AICA stroke requires a systematic approach that integrates clinical expertise with advanced imaging. In my practice, I emphasize the importance of early, objective documentation, as this not only guides acute management but also forms the evidentiary basis for subsequent legal analysis.
Clinical Assessment
The initial evaluation involves a detailed neurological examination, focusing on:
- Cranial nerve function (especially facial movement and hearing)
- Coordination and gait testing
- Sensory and motor assessment
I have found that a thorough symptom chronology—documenting the onset, progression, and combination of vertigo, hearing loss, and facial weakness—can distinguish AICA stroke from mimics such as vestibular neuritis. Clinical assessment should always consider the possibility of overlapping or evolving symptoms, as these may indicate a more extensive infarction as outlined in clinical guidance.
From my unique perspective with both medical and legal training, I can translate complex medical findings into precise documentation that clearly establishes functional limitations for both plaintiff and defense teams. This ability to bridge the medical-legal divide is particularly critical in AICA stroke cases, where subtle distinctions in neurological findings can dramatically impact case valuation.
Imaging and Testing
Definitive diagnosis relies on neuroimaging, particularly:
- MRI with diffusion-weighted imaging to identify acute infarction in the AICA territory
- MR angiography to assess vessel patency
- Audiometry for objective hearing loss documentation
In my experience, early MRI is critical for confirming the diagnosis and excluding alternative causes. Imaging not only localizes the infarct but also provides objective evidence for legal proceedings and rehabilitation planning as supported by research studies.
Having worked with hundreds of spinal cord and brain injury cases, I’ve found that accurate functional assessment and documentation are equally valuable for plaintiffs seeking fair compensation and defendants requiring objective analysis. By ensuring that imaging and clinical findings are described in accessible, precise terms, I help all parties avoid misunderstandings that can compromise either medical care or legal credibility.
AICA Stroke and Legal/Telemedicine Implications
The intersection of AICA stroke with legal and telemedicine considerations is an area where my dual qualifications as a physician and attorney provide unique value. I routinely assist both defense and plaintiff teams in clarifying the medical facts and delineating damages in complex cases.
Expert Medical Analysis
Accurate, contemporaneous documentation of symptoms and findings is essential for both clinical care and legal defensibility. In my experience, the ability to translate nuanced neurological findings into clear, objective language is critical for damage assessment and expert witness testimony. Rehabilitation needs, prognosis, and causation must be addressed with precision, as these factors directly impact the outcome of litigation and insurance claims as highlighted in recent case studies.
While some medical experts focus solely on diagnosis, my approach emphasizes comprehensive functional assessment that provides all parties—physicians, attorneys, and litigants—with clear, accessible documentation of impairments. This strategy not only strengthens the clinical record but also enhances the reliability of expert witness testimony for both plaintiffs and defendants.
To learn how my services combine medical assessment and legal analysis for optimal client outcomes, visit my medical-legal consulting and expert witness services page.
Multi-State Service and Telemedicine Options
Given the rarity and complexity of AICA strokes, access to specialized expertise is often limited. I offer telemedicine consultations and independent medical examinations (IMEs) across multiple states, ensuring that litigants and their counsel receive timely, evidence-based analysis regardless of location. This approach not only expedites care but also supports multi-jurisdictional legal proceedings with consistent, high-quality expert input as recommended in clinical guidance.
By leveraging telemedicine technology, I am able to provide objective, comprehensive evaluations even when in-person access is not feasible—a critical factor for both emergency neurological care and timely legal consultation.
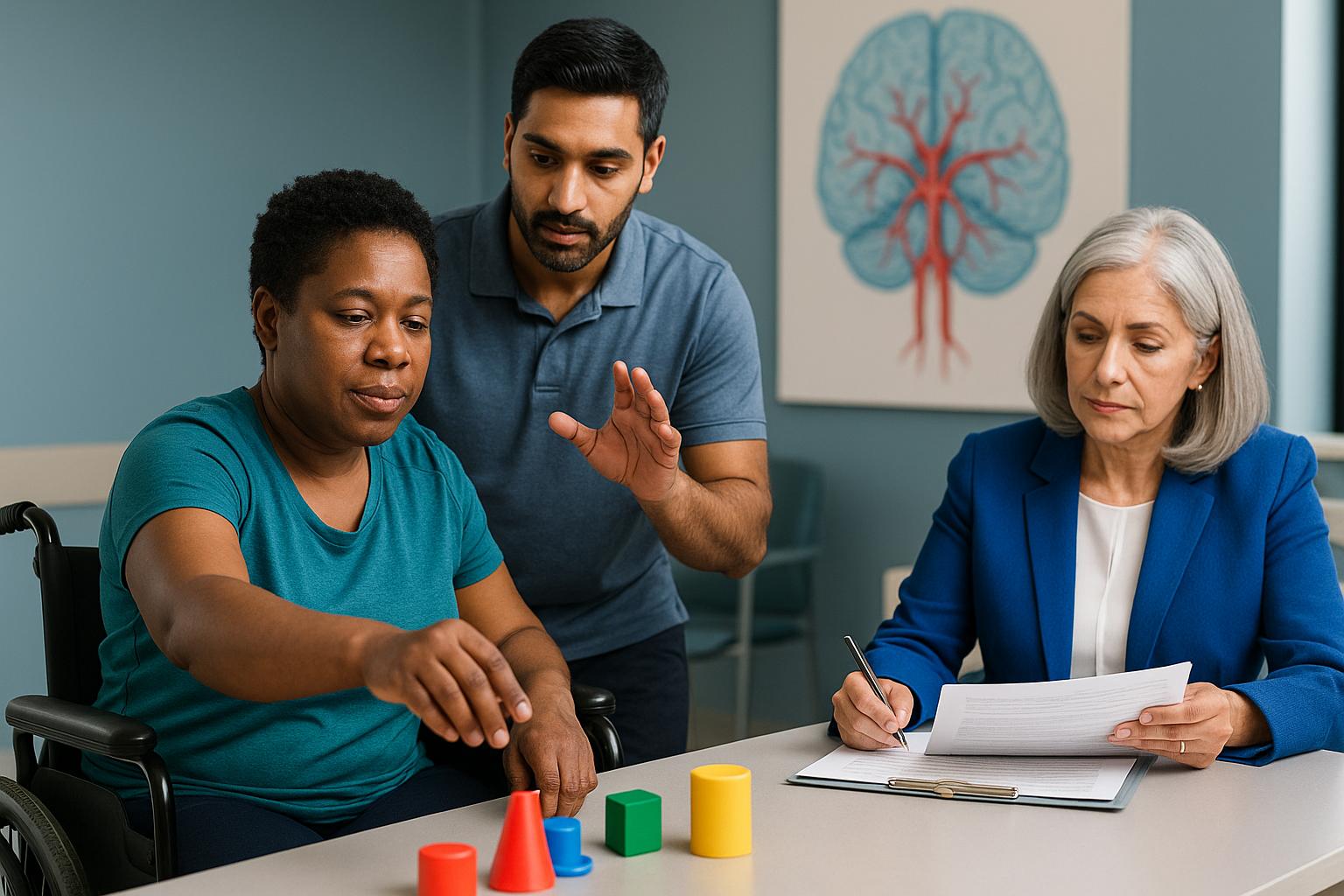
My Approach to Patient Care
Delivering care for individuals experiencing AICA stroke symptoms requires a meticulous, evidence-based approach that integrates both clinical precision and legal clarity. My dual qualifications as a physician and attorney uniquely position me to address the complex intersection of neurological diagnosis and medicolegal documentation.
In my practice, I emphasize the importance of early, objective assessment and comprehensive documentation. This not only guides acute management but also ensures that every aspect of a litigant’s functional impairment is clearly delineated for legal proceedings. My triple board certification in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine allows me to provide nuanced evaluations that are both clinically sound and defensible in court.
I am committed to ongoing professional development, regularly engaging with the latest research and maintaining active licensure across multiple states. This enables me to offer telemedicine consultations and independent medical examinations that meet the highest standards of accuracy and reliability.
Ultimately, my goal is to ensure that every individual—whether patient, attorney, or claims professional—receives clear, actionable insights that support both optimal recovery and fair legal outcomes in cases involving AICA stroke symptoms.
AICA Stroke Symptom Evaluation and Legal Consulting in Reno
As a physician based in Reno, I recognize the unique needs of my local community when it comes to the evaluation and management of AICA stroke symptoms. The region’s diverse population and access to advanced medical facilities make Reno an ideal hub for both in-person neurological assessment and medicolegal consulting.
My practice in Reno is structured to serve not only local patients but also attorneys, claims adjusters, and litigants seeking expert analysis of complex neurological injuries. The city’s proximity to major healthcare centers allows for timely imaging and multidisciplinary collaboration, which is critical for rare conditions like AICA stroke.
In addition to my Reno-based services, I maintain licensure in Texas, California, Colorado, Georgia, Idaho, Montana, North Dakota, Utah, Washington, Pennsylvania, and Kentucky (pending), enabling me to provide telemedicine consultations and expert witness services across multiple jurisdictions. This multi-state reach ensures that individuals and legal professionals throughout the region can access specialized expertise without geographic barriers.
If you are in Reno or the surrounding area and require a comprehensive evaluation of AICA stroke symptoms—whether for clinical care or legal consultation—I invite you to connect with my practice for a virtual second opinion or to request an independent medical examination tailored to your needs.
Conclusion
AICA stroke symptoms—characterized by sudden vertigo, unilateral hearing loss, facial weakness, and balance disturbance—demand immediate recognition for optimal medical and legal outcomes. In summary, timely identification and precise documentation of these rare neurological findings are essential not only for effective treatment but also for establishing a defensible medicolegal record.
My dual qualifications as a triple board-certified physician and attorney uniquely position me to bridge the gap between clinical management and legal clarity, ensuring that both patients and litigants receive comprehensive, objective analysis.
Based in Reno, I provide specialized services across multiple states including Texas, California, and Colorado, and others through both telemedicine and in-person consultations. I am willing to travel as an expert witness when needed, offering flexibility that benefits individuals with complex, multi-jurisdictional cases.
I invite you to schedule a consultation TODAY to secure the best possible medical recovery and ensure thorough legal documentation. Prompt action can make a critical difference in both health outcomes and legal protection, providing you with confidence and peace of mind during challenging times. For more on rehabilitation and recovery guidance, see the latest clinical recommendations.
This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
Frequently Asked Questions
What are the hallmark AICA stroke symptoms?
The hallmark symptoms of AICA stroke include sudden vertigo, unilateral hearing loss, facial weakness, and impaired balance. These symptoms often appear abruptly and may progress over hours. Recognizing this specific combination is crucial, as it distinguishes AICA stroke from more common inner ear disorders and prompts urgent evaluation by a physician.
How can I access your AICA stroke expertise regardless of my location?
You can access my expertise in AICA stroke symptoms through telemedicine consultations and independent medical examinations across all states where I am licensed, including Texas, California, and Colorado. I also offer in-person evaluations and am willing to travel for complex cases or expert witness testimony, ensuring comprehensive care and analysis wherever you are located.
How does your combined medical and legal expertise benefit AICA stroke cases?
My dual qualifications as a physician and attorney allow me to provide both precise clinical assessment and objective legal documentation. This approach ensures that every aspect of a litigant’s functional impairment is clearly delineated, supporting fair and defensible outcomes in both medical recovery and legal proceedings. My experience benefits both plaintiffs and defendants seeking clarity in complex neurological cases.
About the Author
Dr. Ellia Ciammaichella, DO, JD, is a triple board-certified physician specializing in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine. With dual degrees in medicine and law, she offers a rare, multidisciplinary perspective that bridges clinical care and medico-legal expertise. Dr. Ciammaichella helps individuals recover from spinal cord injuries, traumatic brain injuries, and strokes—supporting not just physical rehabilitation but also the emotional and cognitive challenges of life after neurological trauma. As a respected independent medical examiner (IME) and expert witness, she is known for thorough, ethical evaluations and clear, courtroom-ready testimony. Through her writing, she advocates for patient-centered care, disability equity, and informed decision-making in both medical and legal settings.