What is a Hemorrhagic Stroke? A Physician-Led, Patient-Focused Guide
By Dr. Ellia Ciammaichella, DO, JD, Triple Board-Certified in PM&R, SCI, and Brain Injury Medicine
Quick Insights
A hemorrhagic stroke is sudden bleeding in or around the brain, most often caused by high blood pressure or vessel rupture. This dangerous event demands rapid care to reduce brain damage and may carry long-term disability or legal implications.
Key Takeaways
- Hemorrhagic stroke accounts for 10–20% of all stroke cases, with higher rates in some regions according to expert research.
- Major risk factors include uncontrolled hypertension, blood vessel abnormalities, and blood thinners.
- Emergency treatment focuses on stopping the bleed, reducing pressure in the brain, and preventing severe complications.
- Recovery typically involves intensive rehabilitation tailored to each patient’s deficits and future risk assessments.
Why It Matters
Understanding hemorrhagic stroke helps you recognize warning signs, seek emergency care, and prepare for life after stroke. Clear knowledge empowers you to make informed medical and legal decisions that can shape your recovery, protect your rights, and support your loved ones through uncertainty.
Introduction
As a physician with dual expertise in physical medicine and law, I guide patients and families through the complexities of hemorrhagic stroke with both clinical precision and legal insight. You can learn more about my unique background and dual physician-attorney (DO/JD) qualifications here.
Hemorrhagic stroke is sudden bleeding in or around the brain, leading to rapid brain tissue injury that demands immediate intervention and specialized documentation. For individuals in Reno and across multiple states, understanding what a hemorrhagic stroke is essential, not only for urgent care decisions but also for shaping future medical and legal outcomes.
This condition differs fundamentally from an ischemic stroke, as hemorrhagic strokes account for approximately 10–20% of all stroke cases and often result from uncontrolled blood pressure or fragile vessels.
According to current clinical research, the rate of hemorrhagic stroke varies globally, with pronounced effects on long-term disability, recovery expectations, and the need for ongoing rehabilitation. My training as a triple board-certified physician and experience as a legal consultant uniquely position me to clarify both the clinical course and potential legal ramifications of stroke.
Many patients and families confronting a new stroke diagnosis face overwhelming uncertainty—this guide will provide answers, practical support, and a framework for informed decisions.
What is a Stroke?
A stroke is a sudden interruption of blood flow to the brain, resulting in rapid loss of brain function. There are two primary types: ischemic stroke (caused by a blockage in a blood vessel) and hemorrhagic stroke (caused by bleeding in or around the brain). Both types can lead to significant neurological deficits, but their causes, treatments, and outcomes differ substantially.
In my clinical practice, I have seen that recognizing the type of stroke early is critical for determining the most effective intervention. Ischemic strokes are more common, accounting for about 80–90% of cases, while hemorrhagic strokes make up the remaining 10–20%.
Understanding these distinctions is essential for patients and families, as the urgency and approach to care can vary dramatically. Now, let us examine hemorrhagic stroke in greater detail.
Hemorrhagic Stroke: Definition and Overview
A hemorrhagic stroke occurs when a blood vessel in the brain ruptures, causing bleeding that damages brain tissue. This bleeding can happen within the brain (intracerebral hemorrhage) or in the space around the brain (subarachnoid hemorrhage). The sudden increase in pressure can rapidly impair brain function and requires immediate medical attention.
How does a hemorrhagic stroke occur?
Hemorrhagic stroke typically results from chronic hypertension, vascular malformations, or trauma. When a vessel wall weakens or is damaged, it can rupture, leading to bleeding and increased intracranial pressure. In my experience, prompt recognition and intervention are vital to minimizing irreversible brain injury.
As a physiatrist specializing in neurorehabilitation, I place particular emphasis on the importance of timely imaging and nuanced neurological evaluation, as subtle differences in symptoms can influence both acute management and long-term rehabilitation strategies.
Prevalence and statistics
Hemorrhagic stroke accounts for 10–20% of all strokes, with higher rates observed in certain populations and regions. The incidence is notably higher in Asian countries and among older adults. This type of stroke is associated with a higher risk of mortality and long-term disability compared to ischemic stroke. These statistics are supported by robust epidemiological data found in this national stroke research overview.
Ischemic Stroke: Definition and Overview
An ischemic stroke is caused by a blockage in a blood vessel supplying the brain, most often due to a blood clot. This interruption deprives brain tissue of oxygen and nutrients, leading to cell death if not rapidly treated.
Ischemic stroke progression
Ischemic stroke progression can be insidious or abrupt, depending on the size and location of the blockage. Early symptoms may include sudden weakness, speech difficulties, or vision loss. In my practice, rapid diagnosis and intervention—such as clot-busting medications—are crucial for improving outcomes.
From my perspective as a clinician with extensive experience in both acute care and long-term outcomes, I have observed that even small ischemic strokes can lead to significant long-term functional impairment if not addressed promptly. This highlights the need for immediate evaluation and individualized rehabilitation planning.
Global prevalence
Ischemic stroke is the most prevalent type worldwide, accounting for approximately 80–90% of all strokes. Its incidence varies by region, with higher rates in populations with risk factors such as hypertension, diabetes, and atrial fibrillation.
Hemorrhagic vs. Ischemic Stroke: Key Differences
What are the main differences between hemorrhagic and ischemic stroke?
Hemorrhagic stroke is caused by bleeding in or around the brain, while ischemic stroke results from a blocked blood vessel. Hemorrhagic strokes are less common but often more severe, requiring different emergency treatments and recovery strategies.
| Feature | Hemorrhagic Stroke | Ischemic Stroke |
|---|---|---|
| Cause | Blood vessel rupture/bleeding | Blood vessel blockage/clot |
| Prevalence | 10–20% of strokes | 80–90% of strokes |
| Onset | Sudden, severe symptoms | Sudden or gradual |
| Treatment | Stop bleeding, reduce pressure | Suddenly, severe symptoms |
| Recovery | Often longer, more complex | Variable, often faster |
Symptoms comparison
Hemorrhagic strokes often present with sudden, severe headache, vomiting, and loss of consciousness, while ischemic strokes may cause weakness, numbness, or speech difficulties. Recognizing these differences is essential for timely intervention.
In my 15+ years of practice evaluating individuals with spinal cord and brain injuries, I’ve found that detailed functional assessment, beyond basic diagnosis, is essential for accurately delineating the true impact of a stroke—especially when medical-legal clarity is needed.
Treatment and recovery expectations
Treatment for hemorrhagic stroke focuses on stopping the bleed and managing brain pressure, whereas ischemic stroke treatment aims to restore blood flow. Recovery from hemorrhagic stroke is typically more prolonged and may involve greater long-term disability.
While some medical experts focus solely on diagnosis, my approach emphasizes comprehensive functional assessment that provides all parties—physicians, attorneys, and litigants—with clear, accessible documentation of impairments.
Causes and Risk Factors
The causes and risk factors for stroke differ by type but often overlap.
Common causes by stroke type
- Hemorrhagic stroke: Chronic hypertension, aneurysms, arteriovenous malformations, trauma, and blood-thinning medications.
- Ischemic stroke: Atherosclerosis, atrial fibrillation, heart disease, and blood clots.
Having worked with hundreds of stroke and brain injury cases, I have seen that the root causes of stroke can be multifactorial, and identifying these factors is critical for both acute treatment and prevention of recurrence.
Preventable risk factors
- Uncontrolled high blood pressure
- Smoking
- Excessive alcohol use
- Poorly managed diabetes
- Sedentary lifestyle
In my experience, addressing modifiable risk factors through lifestyle changes and medical management is the most effective strategy for reducing stroke risk.
Understanding these risk factors helps guide diagnosis, which we address next.
Common Signs and Symptoms
Recognizing the signs and symptoms of stroke is critical for prompt treatment.
- Sudden severe headache (especially with hemorrhagic stroke)
- Weakness or numbness on one side of the body
- Difficulty speaking or understanding speech
- Vision changes
- Loss of balance or coordination
In my clinical practice, I have observed that early recognition and rapid response can significantly improve outcomes for both stroke types.
When to Seek Medical Attention
Seek immediate medical attention if you or someone you know experiences:
- Sudden severe headache
- Loss of consciousness
- Sudden weakness or speech difficulty
From my unique perspective with both medical and legal training, I can translate complex stroke presentations into documentation that clearly defines the onset and extent of neurological deficits—crucial for subsequent treatment decisions and, when necessary, legal review.
Diagnosis and Assessment
Diagnosing stroke requires a combination of clinical evaluation and advanced imaging.
- CT scan or MRI: To distinguish between hemorrhagic and ischemic stroke
- Blood tests: To assess clotting status and underlying conditions
- Neurological examination: To evaluate deficits and guide treatment
In my role as a triple board-certified rehabilitation expert, I emphasize the importance of rapid, accurate diagnosis to initiate the correct treatment pathway.
In medical-legal cases, comprehensive assessment—including functional ability and long-term prognosis—becomes especially important. I routinely provide these nuanced evaluations for both plaintiffs and defendants, ensuring an objective presentation of the facts.
Treatment Options for Hemorrhagic Stroke
Treatment for hemorrhagic stroke is focused on stopping the bleeding, reducing brain pressure, and preventing complications.
Acute management strategies
- Blood pressure control
- Reversal of anticoagulation (if on blood thinners)
- Surgical intervention (e.g., hematoma evacuation)
- Intensive monitoring in a stroke unit
Current treatment modalities for hemorrhagic stroke primarily involve supportive therapies, with surgical interventions reserved for select cases.
Having worked closely with neurosurgeons and critical care teams, I have observed that individualized treatment—tailored to both the clinical scenario and the patient’s pre-existing health—yields the best outcomes. The decision between surgical intervention and conservative management is complex, requiring multidisciplinary consensus.
Emerging treatments and clinical trials
Ongoing clinical trials are investigating new therapies, including advanced monitoring, novel medications, and cell-based treatments, with details available through current stroke research initiatives. For example, glibenclamide has shown a favorable safety profile but limited functional benefit, with an increased risk of hypoglycemia requiring careful use.
Emerging stem cell-based and regenerative treatments have the potential to influence post-stroke care approaches in the future.
In my experience, participation in clinical trials can offer access to cutting-edge therapies not yet widely available, and having a clear, accessible explanation for both patients and litigants ensures fully informed decision-making.
Recovery and Prognosis
Recovery after hemorrhagic stroke is highly variable and depends on the location and extent of bleeding, as well as the speed of intervention.
- Early, intensive rehabilitation is crucial for maximizing recovery.
- Many patients experience long-term deficits, but multidisciplinary care can improve outcomes.
- Prognosis is generally less favorable than for ischemic stroke, but advances in care are improving survival and function.
My clinical observation is that collaboration among neurologists, physiatrists, and nursing specialists—in a dedicated stroke unit—optimizes both short-term and lifelong outcomes, a fact confirmed by evidence in this multidisciplinary stroke unit research.
Comparing national and international outcomes, I have found that access to specialized rehabilitation services significantly affects recovery, and I advocate for early involvement of physical medicine and rehabilitation from the very beginning of care.
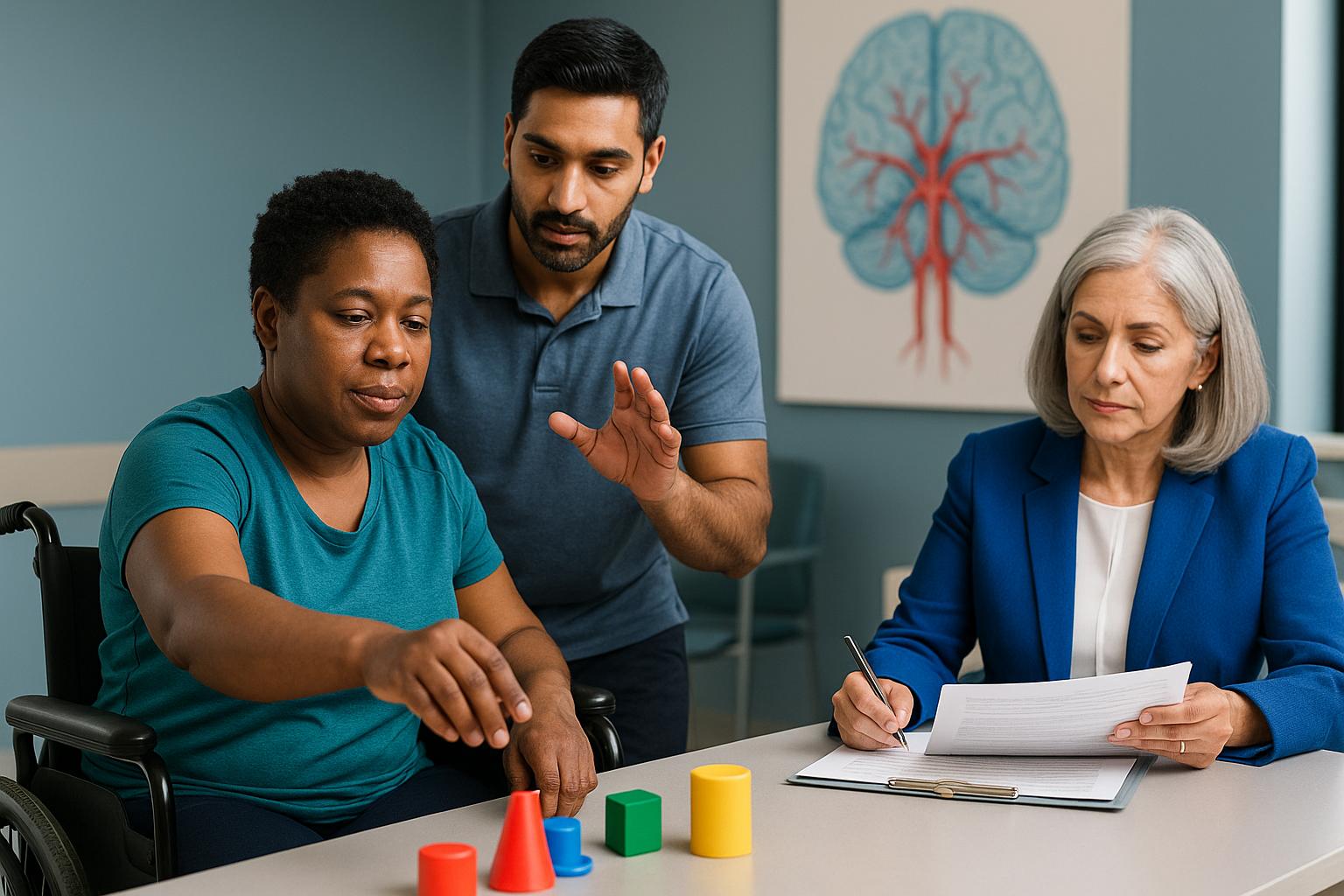
Rehabilitation and Telemedicine Support
Rehabilitation is a cornerstone of stroke recovery, focusing on restoring function and independence.
How rehab aids recovery
- Physical, occupational, and speech therapy tailored to individual needs
- Adaptive strategies for daily living
- Ongoing assessment and adjustment of goals
Research demonstrates that management in a dedicated stroke unit with multidisciplinary care optimizes outcomes, as highlighted by recent clinical trial opportunities.
In my dual role as a physician and legal consultant, I champion intensive, personalized rehabilitation plans that address not just physical deficits, but also cognitive and emotional needs. This holistic approach often makes the difference in whether a stroke survivor regains meaningful independence.
Telemedicine advantages
Telemedicine expands access to expert rehabilitation and follow-up care, especially for those in remote or underserved areas. In my dual role as a physician and legal consultant, I have found that telemedicine not only bridges geographic gaps but also supports continuity of care across state lines.
Additionally, the evolution of clinical trials and tele-rehabilitation programs is accelerating, as outlined in this in-depth research analysis. Being able to coordinate and document care remotely is invaluable, particularly for those whose recovery journey involves multiple providers or legal considerations spanning different locations.
Expert Witness & Legal Consulting Services
My unique qualifications as both a physician and attorney allow me to provide comprehensive expert witness and consulting services for stroke-related cases. I offer objective, evidence-based analysis for both plaintiffs and defendants, focusing on accurate damage assessment and clear, accessible explanations of complex medical concepts.
From my perspective as a dual-degreed DO/JD, I am able to bridge the gap between clinical findings and legal requirements, ensuring that every report or testimony addresses both functional and causation questions with precision.
For attorneys and case managers seeking a trusted partner who understands both the clinical intricacies of stroke and the legal framework of medical litigation, I offer medical assessment and legal consulting services for stroke and brain injury cases. This dual medical-legal expertise ensures clarity, accuracy, and defensible documentation for all stakeholders.
This dual perspective ensures that medical documentation is thorough and that damages are delineated with precision, supporting fair outcomes in litigation and insurance contexts. I am equally comfortable working with legal teams and medical professionals to clarify causation, prognosis, and rehabilitation needs.
My Approach to Patient Care
Delivering care for individuals affected by hemorrhagic stroke requires not only clinical expertise but also a deep commitment to patient-centered advocacy. My philosophy is rooted in the belief that every patient deserves a comprehensive, individualized assessment that addresses both immediate medical needs and long-term functional outcomes.
As a triple board-certified physician in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine, I draw upon years of experience guiding patients and families through the complexities of stroke recovery. My dual training as a physician and attorney enables me to clarify the medical-legal nuances that often arise in these cases, ensuring that both clinical and legal considerations are addressed with precision.
I maintain rigorous standards for documentation, functional assessment, and communication, which are essential for both optimal rehabilitation and clear legal analysis. My ongoing participation in research and professional development ensures that my practice remains aligned with the latest evidence-based guidelines and emerging therapies.
Ultimately, my goal is to empower patients and their families with the knowledge and resources needed to make informed decisions, whether they are navigating acute care, rehabilitation, or legal proceedings related to stroke.
Hemorrhagic Stroke and Stroke Consulting Services in Reno
As a physician based in Reno, I recognize the unique challenges and resources available to those affected by hemorrhagic stroke in this region. The local population may face specific risk factors, such as higher rates of hypertension and limited access to specialized neurorehabilitation, which can influence both the incidence and outcomes of stroke.
My Reno-based practice serves as a hub for both advanced medical assessment and legal consulting, offering in-person evaluations and telemedicine services across Nevada, Texas, and additional licensed states. This approach ensures that patients, attorneys, and local physicians in Reno have direct access to triple board-certified expertise, whether for rehabilitation planning or expert witness consultation.
I am committed to bridging care gaps by providing timely, evidence-based recommendations and supporting local healthcare teams with nuanced functional assessments. For those navigating the aftermath of a hemorrhagic stroke, my practice offers both medical and legal clarity, tailored to the needs of the Reno community and beyond.
If you or your client requires a comprehensive evaluation, a virtual second opinion, or expert witness services related to stroke, I invite you to connect with my Reno office to discuss how I can assist.
Conclusion
A hemorrhagic stroke is a sudden, life-threatening event caused by bleeding in or around the brain, requiring immediate medical intervention and precise documentation. In summary, timely diagnosis, specialized rehabilitation, and comprehensive legal analysis are essential for optimizing both recovery and future legal outcomes.
My dual qualifications as a triple board-certified physician and attorney enable me to address the full spectrum of medical and legal complexities, ensuring that every aspect of your case is managed with expertise and clarity.
Based in Reno, I provide specialized services across multiple states, including Texas, California, and Colorado, and others through both telemedicine and in-person consultations. I am willing to travel as an expert witness, which benefits patients and litigants with complex, multi-jurisdictional cases.
I invite you to schedule a consultation to discuss your case TODAY to secure the best possible recovery and ensure your legal documentation is thorough and defensible. Prompt action can make a critical difference in both your health and your legal peace of mind during this challenging time. For more on current research and evolving standards, see this systematic review of stroke treatment efficacy.
This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard professional medical advice or delay in seeking it because of something you have read in this article. This article does not constitute legal advice or establish an attorney-client relationship. For legal matters, consult a qualified attorney licensed in your jurisdiction.
Frequently Asked Questions
What is a hemorrhagic stroke, and how is it different from an ischemic stroke?
A hemorrhagic stroke occurs when a blood vessel ruptures, causing bleeding in or around the brain. This differs from an ischemic stroke, which is caused by a blocked vessel. Hemorrhagic strokes are less common but often more severe, requiring rapid intervention and specialized care to minimize long-term disability.
How can I access your hemorrhagic stroke expertise regardless of my location?
You can access my expertise through telemedicine consultations in all states where I am licensed, including Texas, California, and Colorado. I also offer in-person evaluations and am willing to travel for complex cases or expert witness needs. This multi-state approach ensures you receive specialized care and legal analysis wherever you are.
How does your combined medical and legal expertise benefit stroke patients and legal professionals?
My dual training as a physician and attorney allows me to provide objective, comprehensive assessments that address both medical recovery and legal documentation. This ensures that all impairments are clearly defined, supporting fair outcomes for plaintiffs, defendants, and attorneys involved in stroke-related cases.
About the Author
Dr. Ellia Ciammaichella, DO, JD, is a triple board-certified physician specializing in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine. With dual degrees in medicine and law, she offers a rare, multidisciplinary perspective that bridges clinical care and medico-legal expertise. Dr. Ciammaichella helps individuals recover from spinal cord injuries, traumatic brain injuries, and strokes—supporting not just physical rehabilitation but also the emotional and cognitive challenges of life after neurological trauma. As a respected independent medical examiner (IME) and expert witness, she is known for thorough, ethical evaluations and clear, courtroom-ready testimony. Through her writing, she advocates for patient-centered care, disability equity, and informed decision-making in both medical and legal settings.