Balance, Vertigo, and Hearing Loss: How AICA Strokes Impact Neurologic Function and Why Early Diagnosis Matters
By Dr. Ellia Ciammaichella, DO, JD, Triple Board-Certified in PM&R, SCI, and Brain Injury Medicine
Quick Insights
Anterior inferior cerebellar artery stroke often leads to sudden vertigo, balance problems, and hearing loss. Studies suggest prompt diagnosis is critical, as symptoms can signal both a medical emergency and potential legal investigation.
Key Takeaways
- AICA strokes can cause rapid-onset dizziness, hearing changes, and unsteady gait.
- The HINTS Plus exam is up to 99.2% sensitive for detecting central causes of vertigo.
- Early intervention improves functional outcomes, with conservative care often preferred.
- Licensed in NV, TX, CA, and more, Dr. Ellia provides expert assessments for complex stroke presentations.
Why It Matters
For attorneys and clinicians, accurately identifying anterior inferior cerebellar artery stroke is crucial—misinterpreted symptoms may delay care or prompt legal scrutiny. Current research indicates timely, expert evaluation can protect patient outcomes and clarify medico-legal responsibility. This answers common pain points around diagnostic uncertainty and case defensibility.
Introduction
As a triple board-certified physician and attorney practicing in Reno, I approach anterior inferior cerebellar artery stroke with both clinical precision and legal insight. My DO/JD background and comprehensive professional experience provide a unique perspective on these complex cases.
Anterior inferior cerebellar artery stroke is a type of posterior circulation stroke that disrupts blood flow to key areas of the brainstem and cerebellum, often resulting in abrupt vertigo, balance issues, and hearing loss.
For both patients and legal professionals, understanding what an anterior inferior cerebellar artery stroke is means recognizing its rapid onset, diagnostic challenges, and the critical importance of timely intervention.
Recent epidemiological research indicates that approximately 795,000 people in the United States experience a stroke each year.
At Ciammaichella Consulting Services, PLLC, I provide expert consulting that bridges Reno’s clinical community and the broader legal landscape, ensuring that every assessment stands up to scrutiny in court and in care.
What Is an Anterior Inferior Cerebellar Artery (AICA) Stroke?
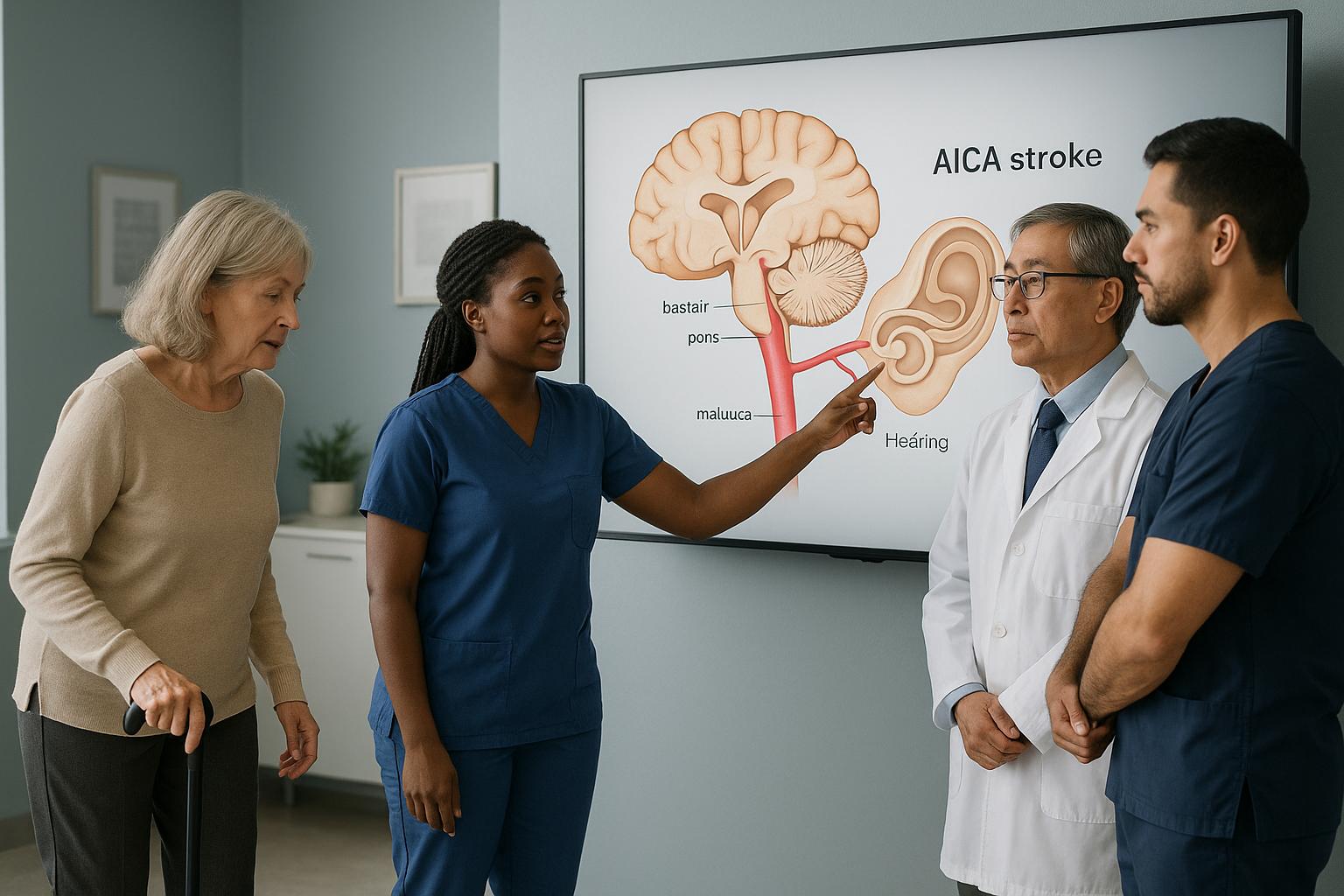
An anterior inferior cerebellar artery (AICA) stroke is a type of posterior circulation stroke that occurs when blood flow through the AICA is disrupted, leading to ischemia in the lateral pons, inner ear, and cerebellum. This event can result in a constellation of neurologic deficits, most notably acute vertigo, hearing loss, and imbalance.
Key symptoms of AICA stroke:
- Sudden vertigo
- Hearing loss
- Unsteady gait or imbalance
- Facial weakness or numbness
- Double vision
AICA Anatomy and Blood Flow
The AICA arises from the basilar artery and supplies critical regions of the brainstem and cerebellum, including the vestibular nuclei and cochlear structures. Disruption of this artery can compromise both auditory and vestibular function, which is why patients often present with combined symptoms.
In my practice, I have found that understanding these anatomical relationships is essential for both accurate diagnosis and effective communication with legal professionals who require precise documentation of injury mechanisms. I recommend this systematic review of AICA variants for a detailed review of AICA anatomy and its clinical implications.
From my unique perspective with both medical and legal training, I can translate complex vascular and functional findings into precise documentation that establishes the full extent of impairment—this is especially critical in cases where subtle differences in anatomy directly affect the symptoms and potential outcomes for litigants.
Epidemiology and Risk Factors
AICA strokes are considered uncommon among posterior circulation events and may be associated with significant morbidity. Common risk factors for stroke include hypertension and diabetes; other factors, such as atrial fibrillation and atherosclerosis, may also contribute.
Epidemiological data indicate that approximately 795,000 people in the United States experience a stroke each year, underscoring the importance of vigilance in both clinical and legal settings. In Reno, I frequently encounter cases where these risk factors are compounded by delayed recognition, which can complicate both medical management and subsequent litigation.
How Do AICA Strokes Affect Balance and Hearing?
AICA strokes uniquely impact both balance and hearing due to the artery’s dual supply to vestibular and cochlear structures. The sudden onset of these symptoms often distinguishes AICA stroke from other causes of vertigo or hearing loss.
Auditory Symptoms: Hearing Loss and Tinnitus
Acute hearing loss, sometimes accompanied by tinnitus (ringing in the ears), may occur in an AICA stroke. This symptom results from ischemia of the inner ear and cochlear nerve. In my experience, the presence of sudden unilateral hearing loss in conjunction with vertigo should always prompt consideration of a central cause, especially in the context of vascular risk factors.
Vestibular Dysfunction: Vertigo and Imbalance
Vertigo—defined as a false sensation of movement—along with severe imbalance, may be observed in AICA stroke. Patients with AICA stroke may exhibit ataxia (loss of coordination) and nystagmus (involuntary eye movements). These findings are critical for differentiating AICA stroke from benign peripheral vestibular disorders.
For residents of Reno, where access to subspecialty care may be limited, recognizing these combined symptoms is vital for timely referral and intervention. I have seen that early identification of these signs can significantly alter both clinical outcomes and the defensibility of medical decisions in court.
In my 15+ years of practice evaluating individuals with spinal cord and brain injuries, I’ve found that detailed functional assessment, beyond basic diagnosis, is essential for accurately delineating damages in legal proceedings. Recognizing the intertwining of auditory and vestibular symptoms is a defining feature of AICA infarcts and should be a central point in any medicolegal analysis.
Recognizing Vestibular Symptoms of AICA Stroke
Distinguishing Central from Peripheral Causes
The challenge in clinical and legal contexts is to differentiate central (brain-based) vertigo from peripheral (inner ear) causes. Central vertigo in AICA stroke may be associated with additional neurologic deficits such as double vision, facial numbness, or severe imbalance.
In my dual role as a physician and legal consultant, I emphasize the importance of a systematic approach to symptom analysis, as misclassification can have profound implications for both patient safety and liability.
Critical Red Flags for Attorneys and Clinicians
Key warning signs that may suggest a central cause include sudden, severe vertigo with hearing loss; persistent imbalance or inability to walk unaided; and associated neurologic symptoms such as facial weakness or diplopia.
For attorneys in Reno and beyond, these red flags are essential for evaluating the standard of care in stroke cases. I routinely advise that any documentation of these symptoms should trigger immediate escalation and, if missed, may become a focal point in litigation.
Based on treating hundreds of patients with brain and cerebellar injury, I’ve found that incomplete assessment of vestibular symptoms is one of the most common reasons for misdiagnosis cited in legal claims. Comprehensive analysis, including both the presence and absence of key neurologic signs, is a cornerstone of my approach to expert review.
When to Seek Medical Attention
If you or your client experiences sudden vertigo, hearing loss, or severe imbalance, seek immediate evaluation by a physician. These symptoms may indicate a stroke and require urgent intervention.
Key Clinical Tests for Diagnosing AICA Strokes
Bedside HINTS Plus Exam
The HINTS Plus exam (Head-Impulse, Nystagmus, Test of Skew, plus hearing assessment) is a bedside tool with up to 99.2% sensitivity for detecting central causes of acute vestibular syndrome, including AICA strokeas outlined in clinical guidelines. The exam includes:
- Head impulse test (assesses vestibulo-ocular reflex)
- Evaluation of nystagmus direction
- Test of skew deviation
- Bedside hearing test
In my practice, I have found that a properly performed HINTS Plus exam can outperform early MRI in identifying posterior circulation strokes, especially when conducted by experienced clinicians.
While some medical experts focus solely on diagnosis, my approach emphasizes comprehensive functional assessment that provides all parties—physicians, attorneys, and litigants—with clear, accessible documentation of impairments. This is particularly crucial when bedside testing influences both immediate clinical decisions and long-term legal analysis.
Role of Imaging in Diagnosis
While MRI with diffusion-weighted imaging is the gold standard for confirming posterior circulation stroke, early imaging can be falsely negative in up to 15% of cases. Therefore, clinical examination remains paramount. For legal professionals, understanding the limitations of imaging is crucial when assessing the timeliness and appropriateness of care. In Reno, I often consult on cases where delayed imaging or misinterpretation has led to adverse outcomes and subsequent legal scrutiny.
Treatment Approaches and Recovery Outcomes
Conservative vs. Surgical Options
Management of AICA stroke typically favors conservative medical therapy, including blood pressure control, antiplatelet agents, and supportive care.
Meta-analyses indicate no significant difference in survival or functional outcomes between conservative and surgical management, with conservative treatment often preferred due to lower risk of severe adverse events. Surgical intervention is reserved for cases with clinical deterioration or life-threatening complicationsaccording to systematic reviews.
Comparing the practical realities of these options, I have observed that conservative management allows for closer monitoring of neurologic function, facilitating adjustment of medications and rehabilitation therapies as indicated. Conversely, surgical intervention is often reserved for severe cases in which there is clear evidence of cerebellar edema or compression.
In the medico-legal setting, documenting decision-making around these inflection points is crucial, as both plaintiffs and defendants rely on a clear explanation of why each pathway was chosen.
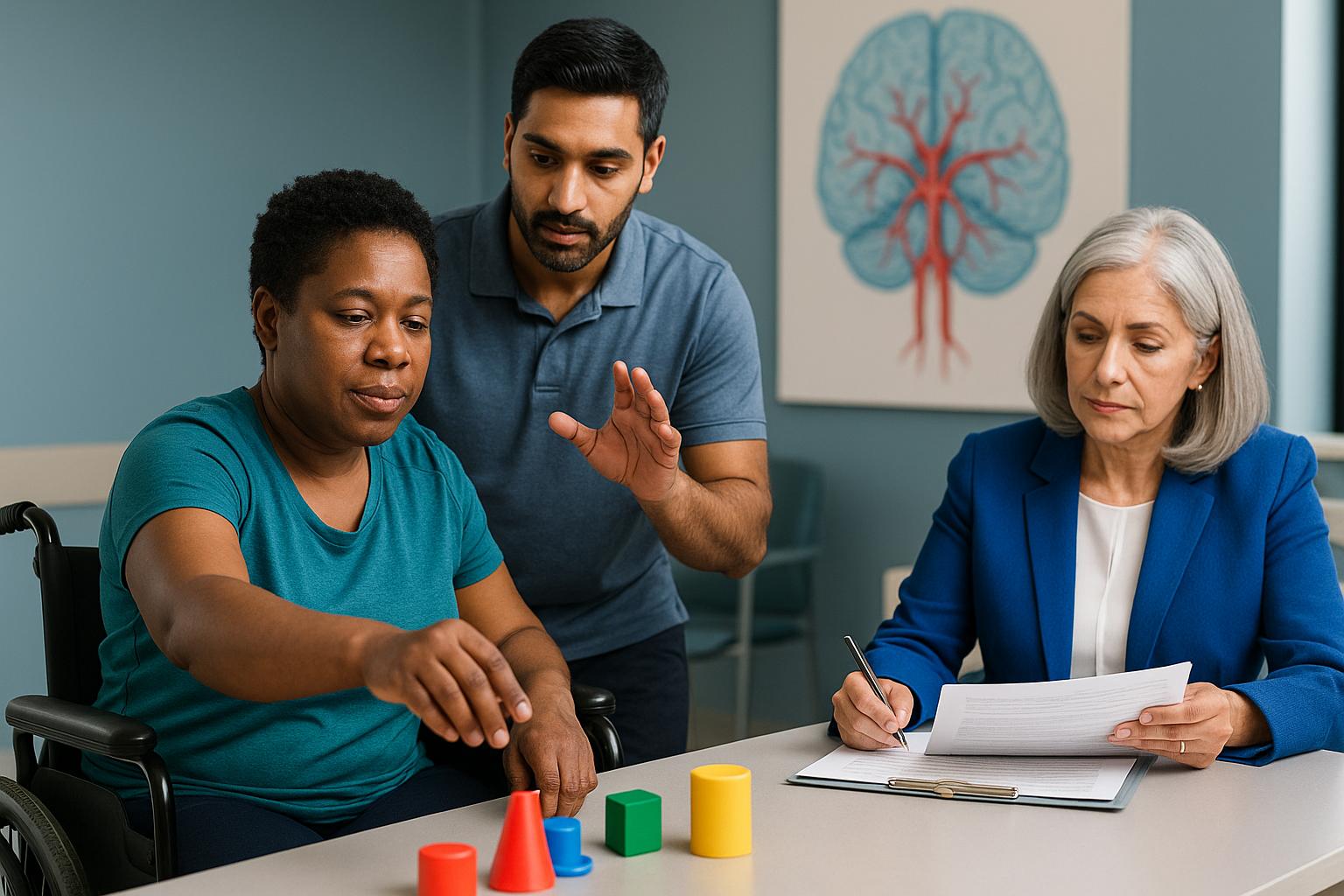
Long-Term Functional Recovery
Most patients with isolated cerebellar stroke, including AICA territory infarcts, achieve favorable long-term outcomes with appropriate conservative management. In my experience, early rehabilitation and multidisciplinary care are critical for optimizing recovery.
For clients in Reno, access to specialized rehabilitation services can make a substantial difference in functional independence and quality of life.
Having worked with hundreds of spinal cord and brain injury cases, I’ve found that accurate functional assessment and documentation are equally valuable for plaintiffs seeking fair compensation and defendants requiring objective analysis.
Recovery trajectories can differ based on the initial severity of the stroke, promptness of intensive rehabilitation, and precise tracking of residual deficits—all elements I carefully outline in medico-legal reports.
Medical-Legal and Telemedicine Expertise Across Multiple States
Expert Witness and IME Services
My dual credentials as a triple board-certified physiatrist and attorney uniquely position me to provide medical assessment and expert witness services for legal cases requiring both clinical accuracy and legal insight. I specialize in translating complex neurologic findings into clear, objective analyses that withstand legal scrutiny.
At Ciammaichella Consulting Services, PLLC, I ensure that every assessment is grounded in current evidence and tailored to the specific medico-legal context.
In summary, from my perspective as a dual-degreed DO/JD with a focus on neurorehabilitation, I am able to close the gap between clinicians and litigants by delivering comprehensive, accessible, and defensible evaluations. This multi-disciplinary expertise benefits both sides of litigation by delineating damages with objectivity and clarity, without serving in a representation capacity.
Telemedicine Reach: Which States Are Covered?
Through telemedicine, I offer stroke consultation and expert witness services across Nevada, Texas, California, Colorado, Georgia, Idaho, Montana, North Dakota, Utah, Washington, Pennsylvania, and Kentucky (pending). For attorneys and clinicians in Reno, this multistate reach ensures access to specialized expertise regardless of location.
I have observed that telemedicine not only expedites expert review but also enhances the defensibility of care decisions in complex stroke cases.
My Approach to Patient Care
Patient experiences are at the core of my commitment to advancing neurologic care, particularly for those facing the sudden and life-altering effects of anterior inferior cerebellar artery stroke. As a physician based in Reno, I have seen firsthand how rapid symptom onset—such as vertigo, hearing loss, and imbalance—can create both medical and legal uncertainty.
My approach is grounded in a meticulous, evidence-based assessment that integrates the latest research with over 15 years of clinical and medico-legal experience. I prioritize clear communication, ensuring that every patient and litigant receives a comprehensive evaluation that stands up to scrutiny in both healthcare and legal settings.
By maintaining triple board certification in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine, I am able to offer nuanced insights that bridge the gap between clinical findings and their implications for functional recovery and legal outcomes. My dual training as a physician and attorney allows me to translate complex neurologic data into actionable recommendations for both medical teams and legal professionals.
Ultimately, my goal is to provide clarity and confidence for individuals and attorneys navigating the challenges of AICA stroke, ensuring that every assessment is both defensible and patient-centered.
Anterior Inferior Cerebellar Artery Stroke Expertise in Reno
Navigating the complexities of anterior inferior cerebellar artery stroke in Reno requires a deep understanding of both the local healthcare landscape and the unique challenges faced by patients and legal professionals in this region. The city’s growing population and diverse risk factors mean that timely, accurate diagnosis and expert consultation are essential for optimal outcomes.
As a physician based in Reno with licensure across multiple states, I am uniquely positioned to provide both in-person and telemedicine consultations for individuals experiencing vertigo, balance issues, or sudden hearing loss. My practice serves as a hub for advanced neurologic assessment and medico-legal analysis, supporting local physicians, attorneys, and litigants who require objective, research-backed evaluations.
Reno’s access to specialized rehabilitation and expert witness services ensures that clients receive comprehensive care and defensible documentation, whether the need is clinical or legal. If you are seeking clarity on complex neurologic symptoms or require an independent medical examination, I invite you to connect with me for a consultation tailored to your needs.
Conclusion
Anterior inferior cerebellar artery stroke is a distinct form of posterior circulation stroke that often presents with sudden vertigo, hearing loss, and balance issues—symptoms that demand immediate clinical and legal attention. In summary, accurate diagnosis and prompt intervention are essential for optimizing medical recovery and ensuring that documentation withstands legal scrutiny.
My dual qualifications as a triple board-certified physician and attorney enable me to provide comprehensive, defensible assessments that address both the medical and legal complexities inherent in these cases.
Based in Reno, I provide specialized services across multiple states, including Texas, California, and Colorado, as well as others, through both telemedicine and in-person consultations. I am willing to travel as an expert witness, ensuring that individuals with complex neurologic presentations receive the highest standard of care and analysis, regardless of location.
I invite you to schedule a consultation TODAY to secure the best possible recovery outcomes and ensure your case is supported by robust, objective documentation. Working with a dual-qualified expert means you benefit from both advanced clinical insight and legal clarity—delivering peace of mind and confidence during challenging times. Prompt action is critical for both health and legal protection.
This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
Frequently Asked Questions
What are the hallmark symptoms of an anterior inferior cerebellar artery stroke?
The hallmark symptoms of anterior inferior cerebellar artery stroke include sudden vertigo, hearing loss, and imbalance. These symptoms often appear abruptly and may be accompanied by facial weakness or double vision. Early recognition is crucial, as timely intervention can significantly improve both medical outcomes and the defensibility of care decisions in legal contexts.
How can I access your expertise if I am not located in Reno?
You can access my anterior inferior cerebellar artery stroke expertise through telemedicine consultations across all states where I am licensed, including Texas, California, and Colorado. I also offer in-person evaluations and am willing to travel as an expert witness. This multi-state practice model ensures that individuals and attorneys nationwide receive specialized, objective assessments for complex neurologic cases.
How does your dual medical and legal background benefit attorneys handling stroke cases?
My combined experience as a triple board-certified physician and attorney allows me to deliver objective, evidence-based assessments that clarify both the medical facts and their legal implications. I provide detailed, defensible documentation that supports fair damage assessment, helping attorneys navigate complex stroke cases with confidence and precision. This approach has been validated through extensive clinical and legal experience.
About the Author
Dr. Ellia Ciammaichella, DO, JD, is a triple board-certified physician specializing in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine. With dual degrees in medicine and law, she offers a rare, multidisciplinary perspective that bridges clinical care and medico-legal expertise. Dr. Ciammaichella helps individuals recover from spinal cord injuries, traumatic brain injuries, and strokes—supporting not just physical rehabilitation but also the emotional and cognitive challenges of life after neurological trauma. As a respected independent medical examiner (IME) and expert witness, she is known for thorough, ethical evaluations and clear, courtroom-ready testimony. Through her writing, she advocates for patient-centered care, disability equity, and informed decision-making in both medical and legal settings.