Understanding AICA Stroke: Causes, Symptoms, and Clinical Evaluation by a Triple Board-Certified Expert
By Dr. Ellia Ciammaichella, DO, JD – Triple Board-Certified in PM&R, Spinal Cord Injury Medicine, Brain Injury Medicine
Quick Insights
AICA stroke is a rare blockage in the anterior inferior cerebellar artery, leading to sudden vertigo, hearing loss, and balance problems. Prompt diagnosis is vital for recovery and can clarify future legal or medical questions.
Key Takeaways
- AICA stroke often causes vertigo, hearing loss, facial weakness, and severe balance issues.
- Symptoms may closely resemble other neurological disorders, requiring careful clinical evaluation.
- Timely identification reduces risk for lasting impairment and supports accurate documentation.
- Available for expert reviews across Nevada, Texas, and other licensed states.
Why It Matters
AICA stroke can be challenging to recognize, confusing attorneys and clinicians alike. Research suggests that missing or mislabeling symptoms can impact both patient outcomes and legal cases. Objective evaluation ensures that care, rehabilitation, and documentation meet the highest standard.
Introduction
As a dual-qualified physician and attorney, I have encountered the diagnostic and legal complexities of AICA stroke in Reno and beyond. To learn more about my unique qualifications as a triple board-certified DO/JD, visit Dr. Ellia Ciammaichella’s professional bio page.
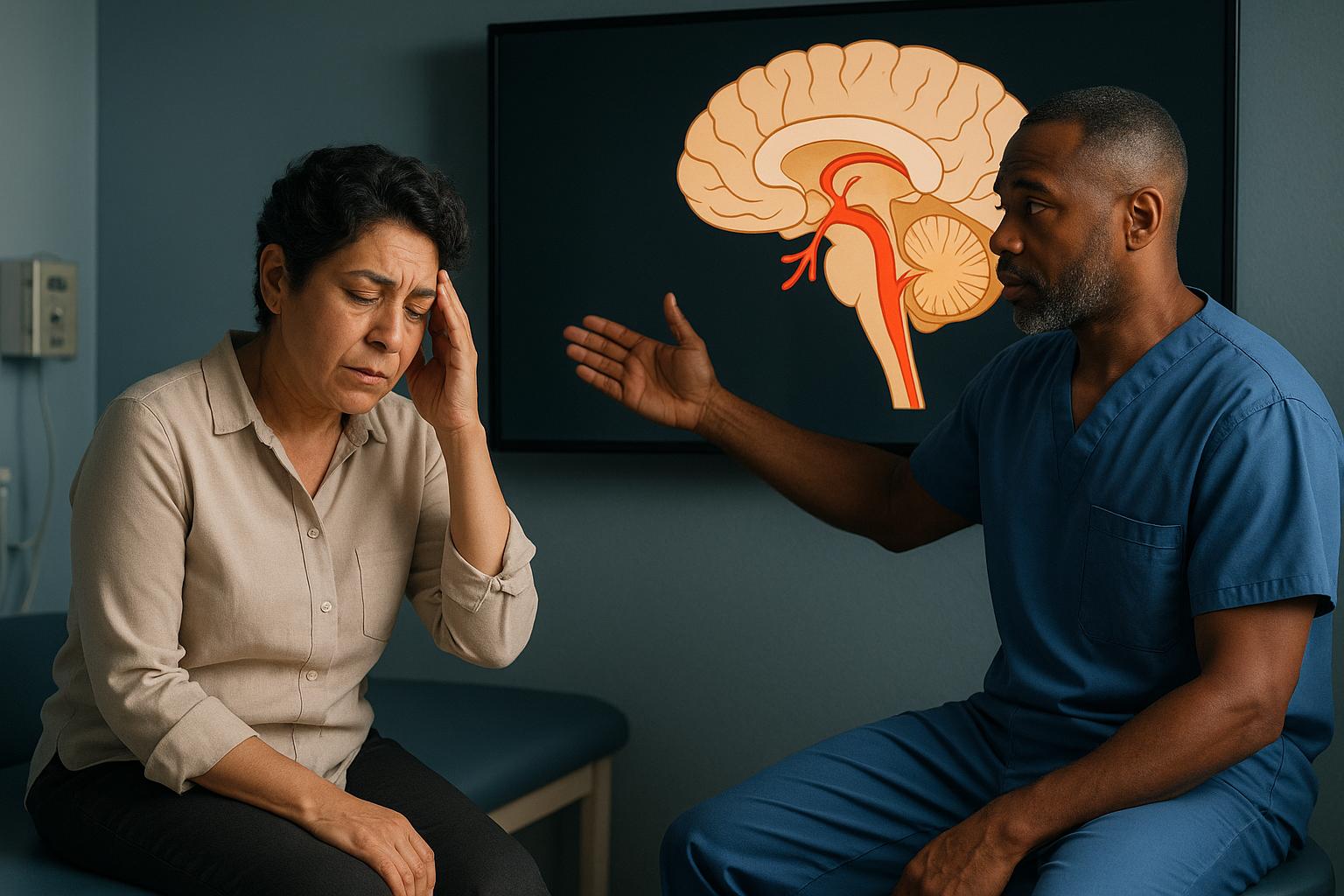
An AICA stroke is a rare ischemic event caused by obstruction of the anterior inferior cerebellar artery (AICA), a vessel supplying the lower brainstem and inner ear. This condition produces acute vertigo, hearing loss, facial paralysis, and severe balance disturbance—symptoms that may closely mimic other neurological disorders.
For both clinicians and litigants, understanding what an AICA stroke is critical, as its recognition determines not only medical management but also the clarity of legal documentation and case outcomes.
My experience in both physiatry and law has shown that objective, well-supported analysis is indispensable for defensible damage assessment. As recent expert guidance emphasizes, precise identification and documentation of AICA stroke symptoms can influence patient recovery and the resolution of complex legal questions.
Accurate, timely evaluation in Reno remains the linchpin for optimal care and robust medico-legal defense.
What is an AICA Stroke?
An AICA stroke is a rare form of ischemic stroke resulting from obstruction of the anterior inferior cerebellar artery (AICA), a vessel supplying the lower lateral pons, inner ear, and parts of the cerebellum. This event deprives critical brain regions of oxygen, leading to sudden neurological deficits.
How does an AICA stroke differ from other strokes?
An AICA stroke uniquely presents with a combination of vertigo, unilateral hearing loss, facial paralysis, and severe balance disturbance. These features distinguish it from more common strokes, which often lack the inner ear and facial nerve involvement seen here.
In my dual role as a physician and legal consultant, I have found that these overlapping symptoms frequently lead to diagnostic confusion, especially in acute settings. In my 15+ years of practice evaluating individuals with spinal cord and brain injuries, I’ve found that detailed functional assessment, beyond basic diagnosis, is essential for accurately delineating damages in legal proceedings.
AICA Stroke vs. Other Strokes
AICA strokes are less common than those involving the middle cerebral artery or posterior inferior cerebellar artery (PICA). The hallmark is the simultaneous involvement of the auditory and vestibular systems, which is rarely seen in other stroke types. This overlap can result in misdiagnosis as benign vertigo or labyrinthitis, delaying appropriate intervention.
Role of Early Recognition
Early recognition of AICA stroke is essential. Prompt diagnosis allows for timely intervention, reducing the risk of permanent deficits.
In my experience, rapid identification and documentation are also crucial for subsequent legal evaluations, as they establish a clear timeline and causation for any resulting impairments. For residents of Reno, where access to specialized stroke care may be limited, awareness of these unique features is particularly important.
AICA anatomy and infarct territory provide further detail on the affected regions.
Causes and Risk Factors
The primary cause of an AICA stroke is a blockage in the anterior inferior cerebellar artery due to a blood clot or atherosclerotic plaque. This event restricts blood flow, resulting in tissue ischemia (oxygen deprivation).
Common Risk Factors
- Hypertension (high blood pressure)
- Diabetes mellitus
- Hyperlipidemia (high cholesterol)
- Smoking
- Cardiac arrhythmias (especially atrial fibrillation)
These risk factors mirror those of other ischemic strokes. In my practice, I have observed that individuals with multiple vascular risk factors are at heightened risk for cerebellar ischemia, including AICA territory infarcts.
Rare Etiologies
Less commonly, an AICA stroke may result from arterial dissection, vasculitis, or congenital vascular anomalies. These rare causes are more challenging to identify and often require advanced imaging for confirmation.
Recent research highlights that the timely identification and treatment of AICA stroke are critical for preventing long-term deficits.
Anatomy: Anterior Inferior Cerebellar Artery
The anterior inferior cerebellar artery (AICA) arises from the basilar artery and supplies the lower lateral pons, inner ear (via the labyrinthine artery), and a portion of the cerebellum.
Damage to this artery disrupts both central and peripheral neurological functions. In my experience, understanding this vascular territory is essential for both clinical and legal professionals, as it explains the unique constellation of symptoms seen in AICA stroke.
From my unique perspective with both medical and legal training, I can translate complex medical findings into precise documentation that clearly establishes functional limitations for both plaintiff and defense teams.
For those in Reno, where regional expertise may be variable, a clear grasp of AICA anatomy can expedite accurate diagnosis and referral.
Detailed AICA anatomy and infarct patterns are available for further review.
Clinical Presentation: How AICA Stroke Manifests
What are the hallmark symptoms of AICA stroke?
AICA stroke typically presents with the following acute symptoms:
- Vertigo (sudden, severe dizziness)
- Unilateral hearing loss
- Facial paralysis or weakness
- Ataxia (loss of coordination)
- Nausea and vomiting
- Gait instability and falls
These symptoms often appear together, making AICA stroke distinct from other stroke types. In my clinical and medico-legal work, I have seen that failure to recognize this pattern can result in missed or delayed diagnosis, with significant consequences for both patient outcomes and legal claims.
Having worked with hundreds of spinal cord injury cases, I’ve found that accurate functional assessment and documentation are equally valuable for plaintiffs seeking fair compensation and defendants requiring objective analysis. The nuances in how symptoms cluster can mean the difference between appropriate intervention and misclassified cases, especially when the stakes involve litigation or insurance questions.
Typical symptoms and clinical features are well-documented in recent literature.
Common Symptoms
- Sudden onset of vertigo
- Hearing loss on one side
- Facial numbness or weakness
- Severe imbalance
Variable/Overlapping Features
Some patients may experience only a subset of these symptoms or present with additional findings such as double vision or sensory changes. This variability complicates the clinical picture, especially in emergency settings.
In my Reno-based practice, I have observed that local clinicians benefit from structured symptom checklists to avoid diagnostic pitfalls.
Balance and fall risk in stroke survivors is a major concern, requiring multidisciplinary management.
When to Seek Medical Attention
If you or someone you know experiences sudden vertigo, hearing loss, or facial weakness, seek immediate evaluation by a physician. These may indicate a serious neurological event requiring urgent care.
Diagnostic Challenges
Diagnosing AICA stroke is inherently complex due to symptom overlap with benign vestibular disorders and other posterior circulation strokes.
In my dual capacity as a physician and legal consultant, I have frequently encountered cases where initial misdiagnosis led to delayed treatment and complicated legal proceedings. An objective, well-documented evaluation is essential for both clinical care and subsequent damage assessment.
While some medical experts focus solely on diagnosis, my approach emphasizes comprehensive functional assessment that provides all parties—physicians, attorneys, and litigants—with clear, accessible documentation of impairments.
Pitfalls in Identification
- Mistaking an AICA stroke for benign vertigo or labyrinthitis
- Overlooking subtle facial weakness or hearing loss
- Incomplete neurological examination
These pitfalls are especially common in busy emergency departments or in regions with limited access to neuroimaging, such as some areas around Reno.
Advanced Imaging/Testing
MRI with diffusion-weighted imaging is the gold standard for detecting cerebellar ischemia. Additional tests may include audiometry and brainstem evoked potentials. In my experience, comprehensive imaging and documentation are indispensable for both treatment planning and legal review.
Early identification and modern treatment strategies are emphasized in current guidelines.
Differential Diagnosis: Distinguishing from Other Cerebellar Ischemia
AICA stroke must be differentiated from other causes of cerebellar ischemia, such as posterior inferior cerebellar artery (PICA) infarcts and vestibular neuritis.
How is AICA stroke distinguished from similar conditions?
AICA stroke is set apart by the combination of vertigo, hearing loss, and facial weakness—features not typically seen together in other stroke types.
Key Similarities
- Both AICA and PICA strokes can cause vertigo and ataxia.
- Overlap with vestibular syndromes may lead to misdiagnosis.
Red-Flag Differences
- Hearing loss and facial paralysis are more specific to AICA stroke.
- PICA strokes rarely involve the inner ear or facial nerve.
In my consulting work, I emphasize the importance of detailed symptom chronology and targeted imaging to clarify the diagnosis. This approach supports both optimal care and robust legal documentation.
From my perspective as a triple board-certified physiatrist with law training, clearly differentiating these syndromes is essential to prevent both medical errors and legal disputes over causation.
Symptom overlap with vestibular syndromes is a recognized diagnostic challenge. Distinguishing clinical features are further detailed in imaging-based resources.
Why Accurate Diagnosis Matters (Clinical and Med-Legal Importance)
Accurate diagnosis of AICA stroke is critical not only for patient care but also for legal and insurance evaluations. As a dual-qualified DO/JD, I am uniquely positioned to bridge the gap between clinical findings and legal standards.
Legal Implications
Precise documentation of symptom onset, progression, and diagnostic steps is essential for defensible damage assessment. In my experience, both plaintiffs and defendants benefit from objective, accessible medical analysis that clarifies causation and the extent of impairment.
I often serve as an expert witness or consultant, ensuring that complex medical concepts are explained in accessible language for all parties. Whether supporting the plaintiff or defense, my role centers on unbiased, comprehensive functional damage assessment that can be clearly presented in court or mediation.
For those seeking a comprehensive overview of both medical assessment and legal applications, learn more about Dr. Ellia’s medical-legal assessment and expert witness services.
Expert documentation and medicolegal standards are foundational for robust case outcomes.
Rehabilitation and Outcome
Timely diagnosis enables early rehabilitation, reducing the risk of long-term disability. For litigants in Reno and beyond, this can significantly impact the calculation of damages and future care needs. My approach always integrates both clinical and legal perspectives to ensure comprehensive, actionable recommendations.
Telemedicine and Multi-State Expert Consultations
My practice offers telemedicine consultations and Expert Medical Consulting Services across Nevada, Texas, and over ten additional states. This model ensures that even clients in remote or underserved areas, such as certain parts of Reno, have access to specialized stroke expertise.
Which States Are Covered?
I am licensed in Nevada, Texas, California, Colorado, Georgia, Idaho, Montana, North Dakota, Utah, Washington, Pennsylvania, and Kentucky (pending). This broad licensure allows me to provide both clinical and medico-legal evaluations across a wide geographic area.
IME and Legal Consultation Process
Clients can expect comprehensive case reviews, medical record reviews, and expert witness testimony tailored to the needs of both legal and medical professionals. In my experience, this integrated approach streamlines the process for attorneys and insurers seeking clear, defensible opinions on complex stroke cases.
Surgical bypass as a treatment option is available in select cases, though most AICA strokes are managed medically.
My Approach to Patient Care
Patient outcomes in rare stroke syndromes such as AICA stroke are profoundly influenced by the precision and thoroughness of the initial evaluation. My practice philosophy is rooted in the belief that every individual deserves a comprehensive, objective assessment that addresses both clinical and legal complexities.
As a triple board-certified physician with dual degrees in medicine and law, I have spent years refining my approach to functional assessment and documentation. This experience allows me to translate intricate neurological findings into clear, actionable recommendations for both medical and legal audiences.
I maintain the highest standards of care by integrating current research, advanced imaging, and detailed symptom analysis. My licensure across more than ten states, including Nevada and Texas, ensures that clients—whether local or remote—receive expert guidance tailored to their unique circumstances.
Ultimately, my goal is to provide clarity and confidence for patients, attorneys, and clinicians navigating the challenges of AICA stroke and cerebellar ischemia. This commitment to excellence is the foundation of my practice and informs every consultation I provide.
AICA Stroke Evaluation and Consulting in Reno
Understanding and diagnosing AICA stroke in Reno requires a nuanced approach, given the region’s unique blend of urban and rural healthcare resources. As a physician based in Reno, I recognize that timely access to specialized stroke expertise can be a challenge for both local clinicians and legal professionals.
I offer comprehensive services that address the full spectrum of AICA stroke, from acute symptom analysis to long-term functional assessment and medico-legal documentation. This dual focus ensures that local clients benefit from both clinical insight and legal clarity, whether seeking a second opinion or preparing for litigation.
If you are in Reno and need specialized evaluation or expert consultation for a complex stroke case, I invite you to schedule a virtual second opinion or request an IME consultation. My expertise is available to support your needs, wherever you are in the region.
Conclusion
An AICA stroke is a rare ischemic event involving the anterior inferior cerebellar artery, often resulting in vertigo, hearing loss, facial weakness, and severe balance impairment. In summary, timely recognition and precise documentation of AICA stroke are essential for both optimal medical recovery and robust legal evaluation.
My dual qualifications as a triple board-certified physician and attorney enable me to bridge clinical and legal perspectives, ensuring that every assessment is both medically sound and legally defensible. Proper care and thorough documentation not only improve patient outcomes but also clarify causation and damages in litigation.
Based in Reno, I provide specialized services across multiple states, including Texas, California, and Colorado, as well as others, through both telemedicine and in-person consultations. I am willing to travel as an expert witness, offering flexibility that benefits clients with complex or multi-jurisdictional cases.
I invite you to schedule a consultation TODAY to secure the most accurate medical assessment and ensure comprehensive legal documentation. Prompt action can make a critical difference in both recovery and legal protection, offering you confidence and peace of mind during challenging times.
This article is for educational purposes only and should not be used as a substitute for professional medical or legal advice, diagnosis, or treatment. Always seek the advice of your physician or qualified legal counsel with any questions you may have regarding a medical condition or legal matter. Never disregard professional advice or delay in seeking it because of something you have read in this article.
Frequently Asked Questions
What are the hallmark symptoms of an AICA stroke?
The hallmark symptoms of an AICA stroke include sudden vertigo, unilateral hearing loss, facial weakness or paralysis, and severe balance problems. These symptoms often appear together and may be mistaken for other neurological or vestibular disorders. Early recognition is crucial, as prompt intervention can significantly improve both medical and legal outcomes.
How can I access your AICA stroke expertise regardless of my location?
You can access my AICA stroke expertise through telemedicine consultations in all states where I am licensed, including Texas, California, and Colorado. I also offer in-person evaluations and am willing to travel for complex cases or expert witness testimony. This multi-state model ensures that clients receive specialized care and objective analysis wherever they reside.
How does your combined medical and legal expertise benefit AICA stroke cases?
My combined medical and legal expertise allows me to provide objective, comprehensive evaluations that address both clinical care and legal documentation. This dual perspective ensures that all findings are clearly explained, causation is well established, and damages are thoroughly delineated—supporting fair outcomes for both plaintiffs and defendants in litigation.
About the Author
Dr. Ellia Ciammaichella, DO, JD, is a triple board-certified physician specializing in Physical Medicine & Rehabilitation, Spinal Cord Injury Medicine, and Brain Injury Medicine. With dual degrees in medicine and law, she offers a rare, multidisciplinary perspective that bridges clinical care and medico-legal expertise. Dr. Ciammaichella helps individuals recover from spinal cord injuries, traumatic brain injuries, and strokes—supporting not just physical rehabilitation but also the emotional and cognitive challenges of life after neurological trauma. As a respected independent medical examiner (IME) and expert witness, she is known for thorough, ethical evaluations and clear, courtroom-ready testimony. Through her writing, she advocates for patient-centered care, disability equity, and informed decision-making in both medical and legal settings.